Search Website
QUICK LINKS:
Curriculum

On this page
Curriculum overview
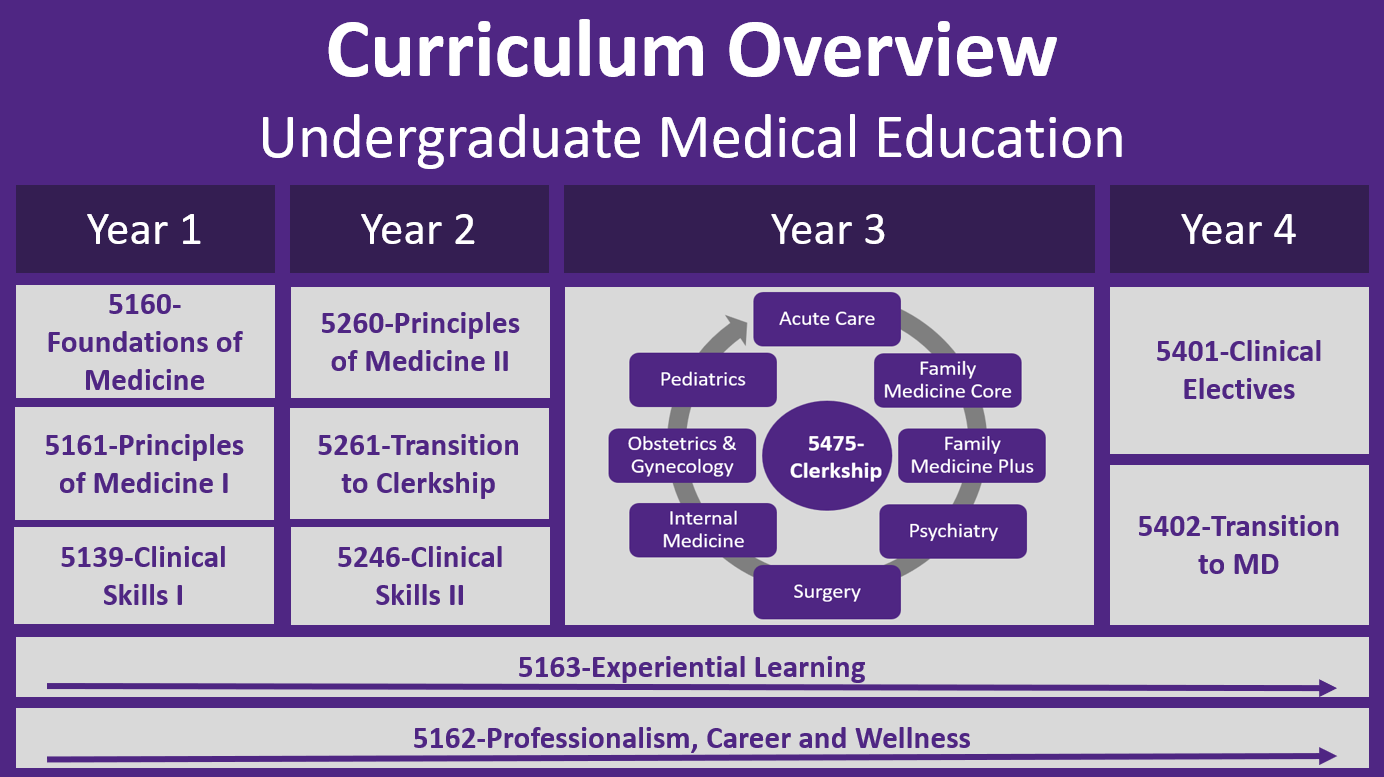
Our four-year medical curriculum integrates early clinical exposure, and hands-on simulation to build strong clinical and diagnostic skills.
Curriculum by year
Learn how we’re transforming our curriculum with a competency-based, patient-informed model designed for today’s complex health care landscape.
Patient-centred approach
Discover how a patient-centered approach shapes our entire curriculum, and encourages a deep understanding of the communities we serve.
Curriculum overview
Our renewed undergraduate medical curriculum embraces a competency-based, active learning approach that supports adaptive, collaborative learning and reflects the evolving needs of care in our communities.
For more information and course descriptions please click on the index buttons above or continue scrolling down this page.
Four year course track:
Curriculum by year
Our four-year MD program provides students with the knowledge, skills and attitudes to advance to graduate or post-graduate studies, leading to clinical practice, research or other medical careers.
Year one
From your first year, you’ ll gain early patient experience through Clinical Methods, where you’ll begin to develop a patient-centred approach to care. At the end of Year 1, you’ll take part in Rural & Regional Discovery Week, working in a hospital or clinic in a Southwestern Ontario community to gain hands-on clinical experience and a deeper understanding of the communities where patients live.
A course taking place from September to the end of December will support and assess learner competence on key topics in the foundational and specific clinical sciences necessary for critical thinking, problem-solving, and clinical decision-making. A key goal is outlined in the first week – “How to think like a physician”.
The curriculum will incorporate the social determinants of health, ethics, cultural competence, health promotion and prevention. This and all subsequent courses will be aligned with issues prominent in Canadian health care, especially those applicable to Southwestern Ontario.
An introduction to Hematology, Infectious Diseases, Immunology and Microbiology will offer clinical application for learning. This course will instill a firm grounding in what will be Themes within courses
Learning will use a variety of methods including case-based and small group/team-based learning, interactive large group learning, labs and independent learning. This course will serve as a secure grounding for learning in other parallel and subsequent Program courses. Students will be introduced to the grounding for EPAs in demonstrating the tasks of a physician.
Year two
Year three
The third year of medicine includes a 52-week integrated Clerkship (Medicine 5475)
The Clinical Clerkship Program at Western’s Schulich School of Medicine & Dentistry is an integrated 52-week course in the third year of the four-year MD program which is distributed across various sites in Southwestern Ontario. During Clerkship, the student becomes an active member of clinical care teams in the following medical disciplines: family medicine, medicine, obstetrics and
The Clinical Clerkship Program in London is being delivered at the Medical Sciences Building and the Dental Sciences Building at Western University, at the London Health Sciences Centre and St. Joseph's Health Care and at other regional education sites through the Distributed Medical Education.
The Clinical Clerkship Program in Windsor is being delivered at the Medical Education Building on the campus of the University of Windsor, at Windsor Regional Hospital, Hôtel-Dieu Grace Hospital and at other regional education sites through the Distributed Medical Education.
The Schulich School of Medicine & Dentistry's Sarnia clerkship program is an immersive, community-based clinical training experience for third-year medical students, established in partnership with Bluewater Health and the Rapids Family Health Team. Students in this new program complete most of their required clerkship rotations in the Sarnia-Lambton area to foster deeper connections and provide a more comprehensive understanding of regional healthcare needs. The program, which began in 2025, includes rotations in various disciplines like family medicine, surgery, obstetrics and gynecology, internal medicince, anesthesia, and emergency medicine. Pediatric rotations are completed at the students' home campus.
Distributed Medical Education includes faculty located in over 45 communities in the region from Tobermory to Leamington. Students learn clinical skills in various geographic sites. The objective is to ensure that Western students at all levels gain an understanding and experience of the practice of
Year four
Beginning in Year 4, Clinical Electives are arranged entirely by the student in any area of medicine, at Schulich Medicine & Dentistry or in other centres. After completion of the Clinical Electives, students return to campus in January for Transition to MD which permits students to further integrate the basic and clinical aspects synthesized with their clinical experience. For more information on 'What You Need to Know' about Year 4 Clinical Electives (including Applying for Electives, Academic/Clinical Policies & Procedures, Assessment and General Information), please click on the link below.
Transition to MD advances student competency beyond Clerkship and is foundational for entering supervised practice. The course supports a learning environment of professional practice to advance Year Four students as mature learners who must be able to function in a learning environment that is grounded in independent learning; small group; collaborative and with some large group interactive non-didactic sessions based on clinical presentations
Patient-centred approach
Learn through a patient-centred curriculum that emphasizes compassion, presence, and a commitment to supporting patients, their families, and communities. Develop the skills to build meaningful relationships with patients, understand their perspectives, and work collaboratively to find shared approaches to care within a broader social and environmental context.
Build a strong foundation in the biological, behavioural, and population sciences, and apply your knowledge in the context of patients’ lives while developing the insight needed to understand their experiences of illness.
Continue the tradition of lifelong learning and discovery shared by all Western MD graduates.