Neuromodulation and Comorbidities in Refractory Epilepsy
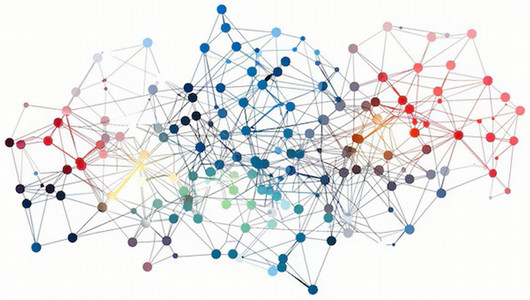
This study focuses on patients implanted with neuromodulation devices (VNS, DBS) as part of their standard care for controlling seizures. The research aims to collect comprehensive data related to epilepsy and outcomes associated with the neuromodulation devices. Participants, or their substitute decision makers, will complete questionnaires before and after implantation, covering quality of life, sleep, headaches, and anxiety-depression. The questionnaires will be collected at baseline, 6 months after implantation, 12 months, 24 months, 36 months, and 48 months. Physiological parameters will be assessed before and after implantation using non-invasive devices during scheduled follow-up clinic appointments. Physiological measures will be collected at baseline, 1 month after implantation, 3 months, 6 months, 12 months, 24 months, 36 months, and 48 months. Patients will also participate in polysomnography and brain MRI for pre-implantation assessment and one year post-implantation. Objectives include identifying outcomes after implantation, recognizing the impact on various aspects of well-being, comparing outcomes before and after implantation, differentiating between VNS and DBS devices, assessing sleep disorders, investigating the impact on the autonomic system, and analyzing the effect on brain connectivity. Consent will be obtained during regularly scheduled clinic visits, with provisions for substitute decision makers. Follow-up questionnaires will also be collected at regularly scheduled clinic visits, telephone and online through REDCAP (pending). This study aims to elucidate the effects of DBS and VNS on multiple aspects of patient well-being, contributing valuable insights for the management of drug-resistant epilepsy and sleep-related disorders.
Inclusion criteria:
- Patients aged 18 to 70 years with drug-resistant epilepsy implanted with a neuromodulation device (VNS, DBS, and RNS).
- Patient or their substitute decision maker able to understand/speak English.
Exclusion criteria:
- Patients who have not been implanted with a neuromodulation device (VNS, DBS, RNS).
- For the 3T brain MRI acquisition, participants would be excluded if they have any of the following conditions: history of head or eye injury involving metal fragments, presence of an implanted electrical or metallic device such as a cardiac pacemaker (this doesn’t apply for the VNS and DBS), if the participant is claustrophobic and/or if there is presence of any metallic implants, such as cerebral aneurysm clips.
Mariam Elnazali (Research Assistant) will obtain initial study consent from patients who have consented to VNS, DBS or RNS surgery. In addition, she will book consenting participants for MRI imaging and a sleep study before and after their surgery, and accompany them to the MRI appointments. Follow-up questionnaires may be collected when patients come for post-surgery appointments. Physiological testing may also be conducted on either the 10th or 7th floor, before and after surgery when patients come in for standard of care clinic appointments. Hannah Gray (PhD student) will conduct physiological testing sessions.
Principal Investigator: Dr. Ana Suller Marti







