Less is More
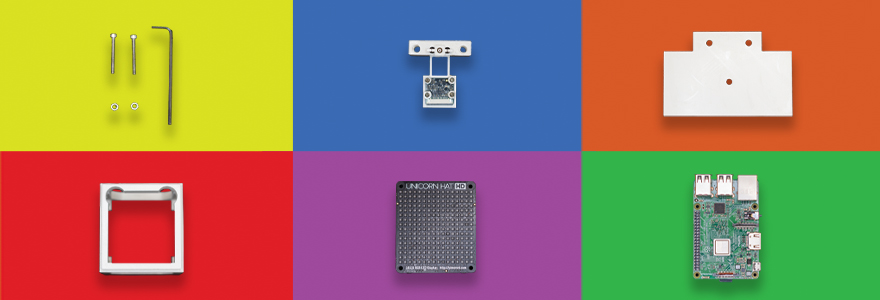 Exploded view of a microscope that identifies malaria.
Exploded view of a microscope that identifies malaria.
COVID-19 showed us how quickly innovation can happen, when demand for traditional medical supplies and devices outstripped supply. What would happen if we applied that same ingenuity and energy to health-care challenges in remote and resource-constrained places?


Top: High-performance intra-oral camera.
Bottom: Low-cost design will help improve dental care.
As three students gathered in a Robarts Research Institute boardroom this summer to discuss their plans for a low-cost oral camera, the lights suddenly flickered and died.
Only the glow of one laptop remained, illuminating their surprised grins. Power outages are rare in this state-of-the-art research building, but in remote and resource-constrained places, intermittent electricity is just one of many challenges that can make providing health care difficult.
“Costs, access to trained professionals, infrastructure challenges – they can all prevent people from getting the care they need in remote places.”
—Tasnia Nabil
“Costs, access to trained professionals, infrastructure challenges – they can all prevent people from getting the care they need in remote places,” said Tasnia Nabil, a recent Western graduate with a medical sciences module, offered by Schulich Medicine & Dentistry. “We’re considering all of these factors in our design for a frugal intra-oral camera to improve dental care in rural Kenya.”
Nabil is among the growing cohort of innovators collaborating across disciplines to fuel medical technology advancements that can improve health care in remote parts of the world.
They’re part of Western’s recently established Frugal Biomedical Innovations program, which is housed at Western Engineering, and backed by Western’s med-tech incubator BioNext, as well as The Africa Institute.
 “In health care, the fanciest gadget is often assumed to be the best thing, and that’s not the same as an efficient and effective solution.”
“In health care, the fanciest gadget is often assumed to be the best thing, and that’s not the same as an efficient and effective solution.”
—Margaret Mutumba, PhD
“In health care, the fanciest gadget is often assumed to be the best thing, and that’s not the same as an efficient and effective solution,” said Margaret Mutumba, PhD, director of the program. “COVID underlined the notion that health care needs innovation and flexibility, especially when facing constraints. That’s what we’re trying to do.”
Biomedical devices are often donated or developed for resource-challenged areas, with little or no consultation with the communities themselves – so they sit on a shelf. Western’s innovators are taking a different approach: One rooted in a true understanding of the community where the innovation is needed.
“To develop truly sustainable biomedical innovations, we must engage with the stakeholders from concept to commercialization,” Mutumba said.
That’s where Melanie Katsivo, PhD, associate director of The Africa Institute, which is housed at Schulich Medicine, comes in. She helps facilitate reciprocal partnerships between university teams and African collaborators – an “essential” step in developing healthcare solutions that meet African priorities and make sense in each country’s landscape.
“We call them ‘equipment graveyards’ – equipment that’s brought to the continent with good intentions, but wasn’t designed with the end user in mind. We’re trying to change that,” she said.
For Nabil’s team, that means developing their low-cost, high-performance oral camera in close partnership with University of Nairobi faculty, dental trainees and care providers – or, as Nabil called them “the experts on the ground.”
Working together, the global team is using LED lights, 3D-printed technology and a low-cost, opensource electronics platform to develop a $300 camera that can identify issues like plaque, cavities and abscesses. In North America, a typical oral camera costs upwards of $3,000.
“In remote regions, this camera can take detailed imagery of a person’s mouth to be sent to a dentist in a city centre, who can then advise on diagnosis, care and treatment,” Nabil said.
“Our microscope can be manufactured for around $200, compared to $10,000 or more for a traditional microscope. At the same time, we’re also improving the microscope’s performance.”
—Justin Yang
One of the defining features of the program is its highly interdisciplinary approach, said James Lacefield, PhD, a professor of Medical Biophysics and Director of Western University’s School of Biomedical Engineering, who helped secure strategic University funding for the initiative.
Dozens of faculty and students from across the University are working shoulder-to-shoulder on diverse frugal innovations, which “helps us and our students become more creative problem solvers, and results in better, more sustainable innovations,” said Lacefield.
Justin Yang is a recent BMSc graduate who started in Schulich Medicine’s MD program this fall. As part of team “ParaSight,” he’s working alongside two Western engineering students, including one with an Ivey Business School background, to develop a low-cost microscope that can diagnose malaria cheaper and more efficiently.
While traditional microscopes use a single light source, ParaSight’s model – which stems from a collaboration with Uganda’s Mbarara University of Science & Technology – uses hundreds of LED lights to capture higher-resolution images of blood smears to identify the malaria parasite using low-cost technology.
“Our microscope can be manufactured for around $200, compared to $10,000 or more for a traditional microscope,” said Yang. “At the same time, we’re also improving the microscope’s performance.”
Yang’s group, under the direction of Ian Cunningham, PhD, a professor of Medical Biophysics, was among 10 Schulich Medicine & Dentistry-affiliated frugal innovation projects that received a boost of up to $30,000 through special grants this summer – from 3D printing hands and legs for people with disabilities to designing a frugal way to measure blood oxygenation to monitor brain injuries in newborns.
 From left, Raymond Li, third-year Software Engineering, Brandon Pautler, second-year Electrical Engineering, and Justin Yang, first-year Medicine.
From left, Raymond Li, third-year Software Engineering, Brandon Pautler, second-year Electrical Engineering, and Justin Yang, first-year Medicine. Microscope design costs about $200.
Microscope design costs about $200. 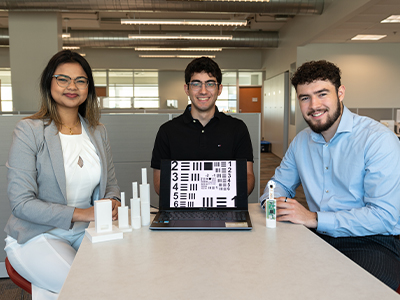 From left, Tasnia Nabil, Schulich Medicine & Dentistry, Fadi El-Richani, Engineering and Jeffrey Donado Visbal, Engineering.
From left, Tasnia Nabil, Schulich Medicine & Dentistry, Fadi El-Richani, Engineering and Jeffrey Donado Visbal, Engineering. While many of the program’s innovators are focused on solutions to improve health care in rural parts of Africa, Mutumba noted the program is designed to support innovations for any remote or resource-constrained part of the world, including Canada.
“Whether we’re innovating to improve health outcomes here or abroad, the same principles apply, and the goal is the same: To contribute to truly sustainable biomedical solutions,” said Mutumba.








