SJHC Based Services
St. Joseph's Operational Stress Injury (OSI) Clinic
Located at the at Parkwood Institute, the St. Joseph’s Operational Stress Injury (OSI) Clinic is part of a national network of ten outpatient clinics funded by Veterans Affairs Canada to provide specialized mental health services to Veterans (and their family), members of the Canadian Forces, and the Royal Canadian Mounted Police (RCMP) with service-related psychological/psychiatric illness. St. Joseph’s OSI Clinic has two satellite clinics located in Toronto and Hamilton. Together, St. Joseph’s OSI Clinic provides service across Ontario including all Southwest Ontario, the Greater Toronto Area (GTA), Hamilton and Niagara region, and portions of Northern and Western Ontario.
The OSI clinic follows a standardized assessment and treatment protocol, including evidence-based psychotherapy and psychiatric care based on clinical practice PTSD guidelines developed by the Canadian Psychiatric Association, the Australian Centre for Posttraumatic Mental Health, the US DVA/DoD and the American Psychiatric Association. The specialized team of psychiatrists, psychologists, nurse practitioners, mental health nurses, and social workers provides comprehensive assessment and treatment in collaboration with community providers. St. Joseph’s OSI clinic has adopted an electronic treatment outcome monitoring system to further enhance treatment outcomes.
Embedded within a clinical and academic centre, the clinic provides training opportunities for learners, medical students, and residents. Community education, outreach, and research are also part of the OSI mandate. Currently there is a combined total of eight psychiatrists (part-time and full-time) working at our St. Joseph’s OSI sites in London, Hamilton and Toronto, all affiliated with the Department of Psychiatry, working predominantly with younger veterans with a geriatric psychiatrist providing psychiatric services for our older veterans population.
Medical Director, Dr. J. Don Richardson states, “St. Joseph’s OSI clinic will continue to strive to improve services and promote research in posttraumatic stress disorder and other operational stress injuries. With the current pandemic our goal is to enhance virtual care to our patients in the community through the Ontario Telemedicine Network (OTN) and other approved formats, improve outreach services to the GTA, Hamilton and Niagara region and further develop training opportunity for residents and psychiatrists interested in veterans’ mental health.”
Collaborative Mental Health Care Services
Overview
A psychiatric consultation team that visits a primary care practice on a regular basis to see and discuss patients, and to provide educational input and advice for primary care providers, has the potential to increase accessibility to psychiatric consultation, strengthen the support for primary care providers, and improve communication between psychiatrists and primary care providers. Such a program is expected to benefit the evolving Southwest Ontario mental health system by enhancing continuity of care, increasing accessibility to mental health services and promoting more efficient use of mental health services, which in other jurisdictions has led to a 46% reduction in the number of cases referred by participating physicians to outpatient services.
Learn more about Collaborative Mental Health Care
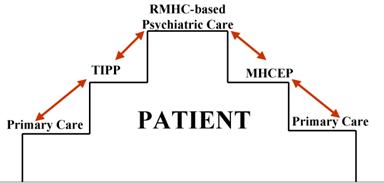
Regional Mental Health Care London (RMHCL) Collaborative Mental Health Care Services
“Stepping up services” and “stepping down services” comprise the two arms of the formal collaborative (shared) mental health care services that have been developed with identified treatment and support providers. Services include treatment, rehabilitation and support interventions to approximately 600 outpatients. RMHC London’s step-up service is named “Mental Health Consultation and Evaluation in Primary-care” (MHCEP). The step-down service is named “Transition into Primary-care Psychiatry” (TIPP). Consistent with a best practices model, program evaluation is an essential component of the MHCEP and TIPP operations. The MHCEP and TIPP program evaluation methodologies were approved by the University of Western Ontario Ethics Review Board.
Contact Us:
| Physician Clinical Team Leader: Dr. Jatinder Takhar, MD, FRCP(C) Collaborative Mental Health Care Services (MHCEP & TIPP) Professor Department of Psychiatry, Western University Phone: 519.455.5110, x.47185 Fax: 519.455.5679 |
Email: Jatinder.Takhar@sjhc.london.on.ca Address: Mood and Anxiety Program, St. Joseph’s Health Care London PO Box 5777, STN B London, ON N6A 4V2 |
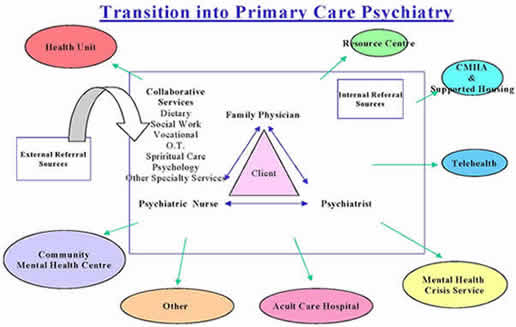
Transition into Primary-care Psychiatry (TIPP)
TIPP, our “stepping down” service, provides transitional treatment and support for clients who are recovering from episodic or other types of mental health services and who are transitioning their care from ambulatory care to care by the primary care physician. The TIPP client base consists of Ambulatory Care clients and Prevention and Early Intervention Program for Psychoses PEPP clients who have maintained a sustained period of wellness and recovery as demonstrated by no significant medication adjustment or need for hospital based care over the last year.
TIPP Description of Service
The TIPP program is based on a modified version of Australia’s Consultation and Liaison in Primary-care Psychiatry (CLIPP) model.
Clients with stable but chronic mental illnesses will be transitioned back to the family physician with assistance from a team consisting of a psychiatrist and a nurse with mental health experience. Other services in the community may be utilized from time to time, according to client need. The model allows for on-site communication between primary care, psychiatry and the client in a least restrictive means with low stigma experience.
The program is unique in that it changes the culture of primary care practice and the balance of power among the team members. Essentially, the model serves as a concept for collaboration between professionals from all fields of health. The TIPP partners include community family physicians, London Health Sciences Centre, Canadian Mental Health Association (CMHA) - London, Western Ontario Therapeutic Communities Hostels (WOTCH), Choice and Opportunities in Rehabilitation and Education (CORE), Middlesex-London Health Unit, London Mental Health Crisis Service, London East Community Mental Health Centre, Telehealth Ontario and other specialty services.
a) Direct consultation
The initial meeting is a face-to-face meeting on site in the family physician’s office with the client/caregiver, if appropriate. At this visit, the transfer summary, relapse signature and medications are reviewed and care is transferred officially to the family physician in primary care practice.
The relapse signature strategy is developed to prevent relapses and recurrences of the client’s illness. This is facilitated as an early intervention strategy in clients at high risk for relapse of their illness. The emphasis is on the wellbeing of the client, prevention of hospitalization, reducing the cognitive effects of the illness on the brain, and maintaining community integration in the various domains. Where possible, members of the client’s family are involved in the preparation of the relapse signature, especially in cases where the client’s symptoms are first noted by his/her family.
b) Indirect services
The nurse visits the family physician at an interval of one to three months while the psychiatrist’s site visits are at intervals of three to six months. These contacts are increased or decreased in frequency depending on the client’s symptomatology, overall functioning, relationships and presence or absence of crises in their lives. During these visits, the client’s progress is reviewed and documented by the team and future management planning is done in a collaborative manner. In between these visits, the family physician maintains the client’s overall status and consults the service as needed. The nurse facilitates timely access to other required services.
Follow-up concerns by consultations, telephone contacts, etc. are documented as indicated. Ongoing assessment during the follow-up is recorded as indicated by the family physician and the psychiatric team. During a follow-up period, the client’s quality of life, symptomatology, functioning in various domains, illness severity and perceived need of care are evaluated, in addition to the team’s level of satisfaction with the model of service delivery.
TIPP Education and Research Activity
Continuing medical education will be provided to the family doctor in an informal peer-to-peer case-based format during the psychiatrist’s and nurse’s regular office visits to the community. The clients’ needs are considered essential in the process so medical education provided to the doctor is relevant in this regard. The educational interventions will be designed as a progression, rather than as isolated programs. Residents and medical students will be encouraged to participate in this teaching and learning model.
TIPP’s research component involves a cluster randomization of a certain group of clients into two treatment arms, “care as usual” and the “TIPP model service care delivery.” The test questionnaire results and subject satisfaction data will be used to evaluate the effectiveness of the overall program. Data that are routinely collected will also contribute to the evaluation of the cost effectiveness of this model of care. The research component will help to solidify the model into clinical practice with supportive evidence.
TIPP Research
Transition into Primary-care Psychiatry (TIPP): A Mental Health Demonstration Project. Funded by The Ministry of Health and Long-Term Care, Primary Health Care Transition Fund. $236,196.60. October 1, 2004 – July 31, 2006; Principal proponents: Drs. D. Haslam and J. Haggarty; Co-proponents: Drs. S. Harris, B. Lent, J. Takhar, C. Dewa, A. Donner, J. Hoch, B. Chaudhuri, J. Goertzen, J. Johnsen.
Transition into Primary-care Psychiatry (TIPP): Assessment of the continuing medical education needs of family physicians providing care to the seriously mentally ill population group within the TIPP model of service delivery. Funded by a Mental Health Grant, St. Joseph’s Foundation. $4,553.00. March 2005 - March 2006. Dr. Jatinder Takhar Principal Investigator, Dr. David Haslam Co-Investigator.
TIPP Publications
Book Chapters
Takhar, J; Haslam, D; McAuley, L; Langford, J. Shared/Collaborative Care for People with Serious Mental Illness. In: A Rudnick and D Roe (Eds), Serious Mental Illness: Person-centered Approaches. (Chapter 5.3). UK: Radcliffe Publishing Ltd. Submitted for publication.
Peer-Reviewed Journals
Takhar, J; Haslam, D; Hobbs, A; McAuley, L. (2010). Enriching relationships through assessment of the Continuing Medical Education (CME) needs of family physicians working within a collaborative care model. Current Psychiatry Reviews, 2010, 6(3):210-218(9). doi: 10.2174/157340010791792635
Haggarty, J; Haslam, D; Houlding, C; Armstrong, D. (2008). Clinical findings of a cluster randomised control pilot trial of a Canadian Shared Care service for those with chronic mental illness. Primary Care and Community Psychiatry, 13(1):19-25(7). doi: 10.1080/17468840801890060
Haggarty, J; O'Connor, B; Dubois, S; Blackadar, AM; McKinnon, T; Boudreau, D; Haslam D. (2008). A pilot study of a Canadian shared mental health care programme: Changes in patient symptoms and disability. Primary Care and Community Psychiatry, 13(1):27-35(9). doi: 10.1080/17468840801892645
Haslam, D; Haggarty, J; McAuley, L; Lehto, J. Takhar, J. (2006). Maintaining and enhancing shared care relationships through the TIPP clinical model. Families, Systems & Health, 24(4):481-486. doi: 10.1037/1091-7527.24.4.48
Abstracts/Presentations
Baird, K; Takhar, J; Haslam, D; McAuley, L; Finigan, A; Langford, J. (June 19, 2008). Development of a process for quality control through chart review within the context of a Transition into Primary Care Psychiatry (TIPP) program. Poster at Annual Research Day, Department of Psychiatry, University of Western Ontario, London, Ontario.
Bush, H; Langford, J; Jackson, L; Takhar, J; et al. (May 29, 2009). Shared care services to indigent populations in London, Ontario, 2004-2008. Poster at National Conference on Collaborative Mental Health Care, Hamilton, Ontario.
Haggarty, J; Haslam, D; Takhar, J. (May 20-25, 2006). A tale of two cities: Lessons learned from research protocol variance. Poster at American Psychiatric Association Annual Meeting, Scientific Program, Toronto, Ontario.
Haggarty, J; Haslam, D; Takhar, J. (May 11-13, 2006). A tale of two cities: Lessons learned from research protocol variance. Poster at 7th National Conference on Shared Mental Health Care, Calgary, Alberta.
Haslam, D; Haggarty, J; Kolisnyk, G; Caruso, R; McAuley, L; Lehto, J; Dunbar, S; Takhar, J. (Sept 20, 2006.) Transition into Primary-care Psychiatry (TIPP): Perceived need for care and participant satisfaction outcomes. Primary Healthcare Network Symposium, Vancouver, British Columbia.
Haslam, D; Haggarty, J; Kolisnyk, G; Caruso, R; McAuley, L; Lehto, J; Dunbar, S; Takhar, J. (May 11-13, 2006.) Transition into Primary-care Psychiatry (TIPP): Perceived need for care and participant satisfaction outcomes. 7th National Conference on Shared Mental Health Care, Calgary, Alberta.
Haslam, D; Haggarty, J; Takhar, J. (May 23, 2006). Transition into Primary-care Psychiatry (TIPP): The feasibility of conducting a full-scale cluster randomization study. Poster at the American Psychiatric Association 159th Annual Meeting, Scientific Program, New Research, Toronto, Ontario.
Haslam, D; Haggarty, J; Takhar, J. (May 11-13, 2006). Transition into Primary-care Psychiatry (TIPP): The feasibility of conducting a full-scale cluster randomization study. Poster at 7th National Conference on Shared Mental Health Care, Calgary, Alberta.
Haslam, D; Haggarty, J; Takhar, J; Caruso, R; Kolisnyk, G. (May 11-13, 2006.) It's about the patient: going beyond the satisfaction questionnaire: research on clients' experiences in a shared mental health care model. 7th National Conference on Shared Mental Health Care, Calgary, Alberta.
Haslam, D; Haggarty, J; Takhar, J. (Nov 3-6, 2005). Transition into Primary-care Psychiatry (TIPP). 55th Annual Conference of the Canadian Psychiatric Association, Scientific Program, Vancouver, British Columbia.
Haslam, D; Takhar, J; Dixon, D. (May 29, 2009.) Depression education and enhancement in primary (DEEP) Care. Poster at National Conference on Collaborative Mental Health Care, Hamilton, Ontario.
Lehto, J; McAuley, L; Melville, S; Haggarty, J; Takhar, J; Haslam, D. (May 15, 2007). TIPP clinical findings from the third year in expanding collaborative relationships. Poster at Regional Mental Health Care London and St. Thomas 8th Annual Research Half Day, St. Thomas, Ontario. (abstract in Research Insights).
Lehto, J; McAuley, L; Takhar, J. (June 10-11, 2005). TIPP clinical findings from the first year in maintaining and enhancing shared care relationships. Poster at 6th National Conference on Shared Mental Health Care, Ottawa, Ontario.
McAuley, L; Lehto, J; Haslam, D; Haggarty, J; Takhar, J. (April 2006). Transition into Primary-care Psychiatry (TIPP): Clinical findings from the first year in maintaining and enhancing shared care relationships. Poster at 19th Annual Research Conference University of Western Ontario School of Nursing, London, Ontario.
McAuley, L; Lehto, J; Takhar, J. (May 11-13, 2006). TIPP clinical findings from the second year in sustaining collaborative relationships. Poster at National Conference on Shared Mental Health Care, Calgary, Alberta.
Takhar, J; Hobbs, A; Haslam, D; McAuley, L. (June 7-9, 2007). Transition into Primary-care Psychiatry (TIPP): Assessment of the continuing medical education needs of family physicians providing care to the seriously mentally ill population group within the model of service delivery. Poster at 8th National Conference on Collaborative Mental Health Care, Quebec City, Quebec.
Takhar, J; Hobbs, A; Haslam, D; McAuley, L. (May 15, 2007). Transition into Primary-care Psychiatry (TIPP): Assessment of the continuing medical education needs of family physicians providing care to the seriously mentally ill population group within the model of service delivery. Poster at Regional Mental Health Care London and St. Thomas 8th Annual Research Half Day, St. Thomas, Ontario.
Takhar, J; Hobbs, A; Haslam, D; McAuley, L. (Oct 5, 2006). Transition into Primary-care Psychiatry (TIPP): Assessment of the continuing medical education needs of family physicians providing care to the seriously mentally ill population group within the model of service delivery. Poster at GAMES Education Symposium, London, Ontario. (abstract in Research Insights)
Takhar, J; McAuley, L; Finigan, A; Langford, J; Haslam, D; Baird, K. (May 17, 2008). Development of a process for quality control through chart review within the context of a Transition in Primary Care Psychiatry (TIPP) program. Poster at 2008 National Conference on Collaborative Mental Health Care, Victoria, British Columbia.