Schulich Medicine research leads to new understanding of how HIV hides itself in the body
By Prabhjot Sohal
When the human immunodeficiency virus (HIV) infects a person’s body, it permanently inserts its genetic material into the genome where it often remains dormant and barely detectable for years. A major obstacle in finding a cure for HIV has been solving the mystery of how this dormant pool of HIV-infected cells, also called HIV latency, is established.
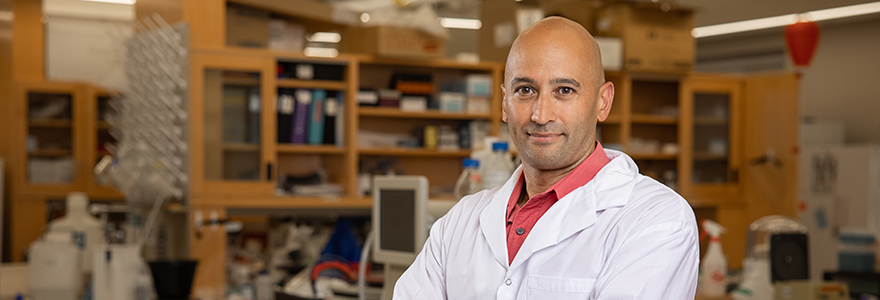
A new joint study led by Stephen Barr at Schulich School of Medicine & Dentistry and University of Ottawa’s Marc-André Langlois has identified a new function of a virus-fighting protein called APOBEC3 (A3) in the integration process of HIV in the human genome.
The study, published in Nature Communications, has found that APOBEC3 proteins — which are responsible for generating mutations in the genetic material of HIV in an attempt to kill the virus — can redirect the integration of HIV into less active regions of the genome.
“Normally, APOBEC3 proteins are very efficient at generating lethal mutations in the HIV genome. However, HIV has a protein that significantly lowers the levels of APOBEC3, allowing the virus to escape destruction and insert its genetic material into the human genome to establish infection,” said Barr, professor of microbiology and immunology at Schulich Medicine. “In our study, we showed that when APOBEC3 proteins are unable to completely destroy the HIV genome, they try to hide it in a ‘dark’ place in the human genome where the virus cannot produce new viruses, as a last-ditch effort to silence the virus. While this safe place allows the virus to go undetected for many years, eventually it can still awaken and cause disease.”
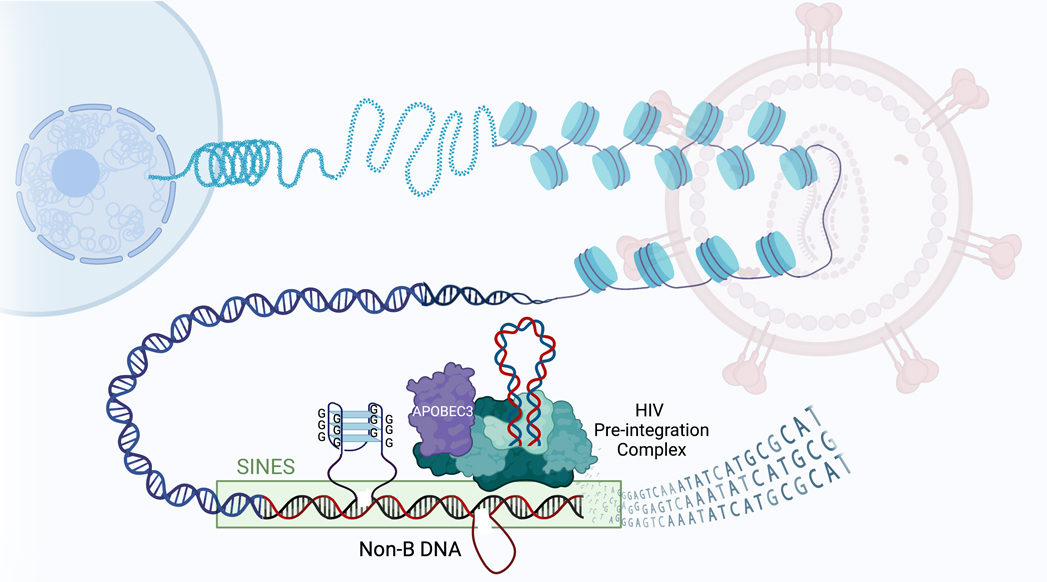 Graphical abstract representing how APOBEC3 plays a role in HIV latency. (Stephen Barr)
Graphical abstract representing how APOBEC3 plays a role in HIV latency. (Stephen Barr)
In this way, Barr says the study has identified APOBEC3 as a new player in the integration of the HIV genome into the human genome and a potential key factor in the establishment of HIV latency.
The researchers say this study has also identified a potential key to eliminating HIV through this function of APOBEC3 proteins and helps scientists better understand the establishment of life-long HIV infection, which could lead to the development of more effective therapeutics to eliminate HIV from the body.
“We can keep HIV under tight control with antiretroviral drugs – and those drugs work wonderfully. But they’re not a cure. We are striving for a cure, and we think part of the countermeasures following an exposure will be to block the activity of these A3 proteins to inhibit HIV latency,” said Marc-André Langlois, professor at the University of Ottawa Faculty of Medicine and Chair in Pandemic Viruses and Preparedness Research.
“We’ve done the first demonstration that this mechanism—something that wasn’t on the radar and goes against mainstream thought—is really happening. So, this is the first layer of evidence, and we’ll be building on it with follow-up studies,” said Langlois.








