Feature: Simulation improves care, confidence during COVID-19

By Emily Leighton, MA'13
A woman in preterm labour with a confirmed case of COVID-19 arrives at the hospital.
From the screening process at the front entrance to delivering the baby and transferring the mother to critical care, health care providers and frontline staff must carefully and strategically manage the situation.
Coordination is essential – even pushing elevator buttons invites the risk of contamination.
This scenario played out during a recent hospital-wide obstetrics simulation performed at London Health Sciences Centre (LHSC). “We can close a lot of elective services, but we can’t close OB,” said Dr. Rob Leeper, MD’07, Assistant Professor with the Department of Surgery. “People still have babies during a pandemic.”
More than 30 Schulich Medicine & Dentistry faculty members are engaged in creating and delivering interprofessional simulation experiences, with the goal of helping health care providers learn, adapt and prepare for the COVID-19 cases they may encounter.
The obstetrics simulation, led by Dr. Taryn Taylor, MD’10, Assistant Professor with the Department of Obstetrics and Gynaecology, was one of about 50 COVID-19 simulations that have taken place, with more planned.
“Simulation has always been considered an important tool for health care providers. Highly realistic practice and timely feedback on performance are how individuals and teams improve,” said Dr. Rich Cherry, MD’93, Associate Dean of Learning with Technology & Simulation. “This is even more important in unprecedented times such as this. COVID-19 has changed enormously the way patients need to be cared for and the action of teams responsible for their care.”
Many of the simulations are happening in real clinical environments with real equipment, known as in-situ simulation. Importantly, simulations are being modified in accordance with conservation strategies and policies for personal protective equipment.
“Simulation provides a unique opportunity to bridge the gap between policy, education and practice,” said Dr. Taylor, who is also a Scientist with the Centre for Education Research & Innovation at the School. “It enables agility, particularly in times of crisis, when policies are changing daily and teamwork is more important than ever.”
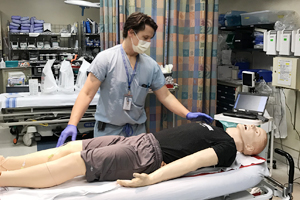 Dr. Leeper, a trauma surgeon, recently led a comprehensive in-situ trauma simulation for a patient with a gunshot wound who had just crossed the border from the United States and had tested positive for COVID-19. The team included paramedics, nurses, critical care physicians, surgeons, respiratory therapists and x-ray technicians.
Dr. Leeper, a trauma surgeon, recently led a comprehensive in-situ trauma simulation for a patient with a gunshot wound who had just crossed the border from the United States and had tested positive for COVID-19. The team included paramedics, nurses, critical care physicians, surgeons, respiratory therapists and x-ray technicians.
During the debriefing phase, the team looked at how much personal protective equipment was affected and how much contamination took place within the trauma bay. The simulation was also observed by staff from the hospital’s cleaning service, who provided important feedback on loss of supplies due to contamination and cleaning time to make the room usable again.
“It was really eye opening,” said Dr. Leeper. “From this one scenario, we’re now suggesting changes in air controls and rapid changes to the physical layout of the trauma area, putting up physical barriers to improve our ability to contain aerosolized contagion.”
As an anesthesiologist, Dr. Cherry is focused on airway management and intubation for patients with confirmed or suspected COVID-19 – one of the highest-risk moments in care. Initial lessons have included the need for a checklist when donning and doffing personal protective equipment and a second person spotting its removal, as well as adjusting the ergonomics of the operating room to minimize cross-contamination of equipment.
“A pandemic is new for everyone, including health care providers,” said Dr. Cherry. “Simulation lets us observe teams in action, receive their input about how the processes and procedures seem to perform and then rapidly adjust our approaches as needed. Everyone feels far more confident and more at ease if they have the opportunity to practice before a true crisis presents.”
By focusing on changes in behaviour and the physical environment, simulation is improving patient care while also helping health care workers cope with uncertainty and anxiety.
“There are so many things that are beyond our control,” explained Dr. Leeper. “Simulation gives us the chance to do something, to learn about ourselves and to teach each other. That is really meaningful and empowering at a time like this.”








