Breaking down barriers
By Max Martin, MMJC’19
Cost, fear and even proximity to clinics are just a few of the barriers that can prevent Canadians from accessing dental care.
“The first barrier to dental care is cost, there is no question about that,” said Dr. Kenneth Wright, adjunct faculty member and founder of the School’s Dental Community Outreach Service (DOCS) program. “But then there are other barriers too.”
Unfortunately, the list goes on, with factors like fear of health care institutions and white coats, lack of availability of services in isolated regions, or other mental and physical health challenges hindering millions of Canadians from visiting a dentist. A lack of understanding of the role of oral health and overall health can also be a contributing factor.
Nearly 35 per cent of Canadians do not have dental insurance.
In 2018, 22.4 per cent of Canadians, or 6.8 million, reported avoiding going to the dentist because of cost.
Among the countries poorest, that number rises to just shy of 50 per cent not seeing a dentist due to the expense.
So how do you solve a multifaceted, complex socioeconomic problem? Faculty and learners at Schulich Dentistry are pointing to community outreach and grassroots initiatives to help bridge the gap in dental care and break down barriers that prevent individuals from visiting the dentist.
Community Affordable Dental Clinic
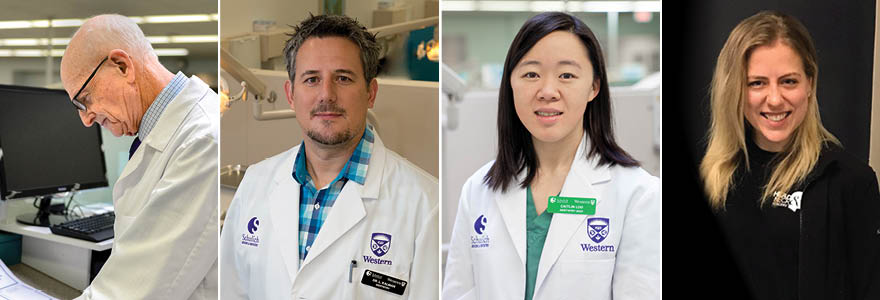
Dr. Wright has been pioneering accessible dental care for decades.
Now, his latest venture could be one of the most impactful yet – London, Ontario’s first brick-and-mortar affordable dental clinic.
Located above the Glen Cairn Community Resource Centre on Adelaide Street, the clinic will service low-income Londoners throughout the city.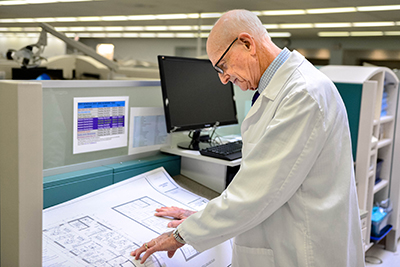 “The need in London is pretty high,” said Dr. Wright, citing upward of 70,000 Londoners living at or below the poverty line and nearly 100 monthly visits to the emergency room for dental emergencies.
“The need in London is pretty high,” said Dr. Wright, citing upward of 70,000 Londoners living at or below the poverty line and nearly 100 monthly visits to the emergency room for dental emergencies.
Run by the London Community Dental Alliance, a non-profit made up of community organizations and stakeholders, the clinic will house four dental chairs and bring together a team of full-time dentists and hygienists. Dr. Wright said the clinic is also counting on additional dentists and practitioners to volunteer their time at the clinic throughout the year.
The clinic aims to serve between 4,000 and 5,000 appointments each year. The goal is to open the clinic early in the summer of 2020.
A key feature of the facility will be a part-time navigator position – a role designed to break-down the various barriers faced by individuals seeking affordable dental care.
“Unfortunately, outreach work tends to suffer from a high no-show rate,” said Dr. Wright. The navigator will work to close this gap, identifying the needs of patients to get them into the clinic.
“The other challenge is in meeting the complex needs of marginalized populations,” Dr. Wright explained. “Often, these patients haven’t been to a dentist in years or maybe have never seen a dentist. So, their mouths are in terrible shape, which can require multiple appointments and more time to treat.”
And while he’s dedicated most of his life to dentistry and community outreach, Dr. Wright shows no signs of slowing down.
“I’ve been retired for 20 years. Some people take up woodwork, but I’ve always been involved in volunteering, so heading this up seemed to be a natural fit.”
As for breaking down larger socioeconomic barriers to accessible dentistry, Dr. Wright says enhancing current and driving future community outreach is the first step.
“Grassroots initiatives are essential,” Dr. Wright said on making dentistry more accessible. “I don’t see how else you’d do it. My hope would be if we can make this work, then there might be more in the city of London one day.”
Dental Community Outreach Service
The DOCS program has been a hallmark of Schulich Dentistry for more than a decade. Offering free dentistry to low-income patients, the clinic – a mandatory part of the fourth-year curriculum and the Internationally Trained Dentists program – helps provide dental care to some of those most in need.
“There has always been a need here in London,” said Dr. Les Kalman, Chair of the DOCS program. “Going into the community, I think there is an even bigger need, and maybe the disparities are bigger in oral health and in wealth. That’s a challenge.”
Having grown up in London, Dr. Kalman feels a greater connection to the city he calls home, and the role his outreach can play. “It hits home how real this problem is. It’s been twice now at a clinic where a patient has come up and thanked me, and we went to the same high school. That’s a really weird feeling,” explained Dr. Kalman. “If I didn’t grow up in this environment, I think my perspective would be very different.”
“It hits home how real this problem is. It’s been twice now at a clinic where a patient has come up and thanked me, and we went to the same high school. That’s a really weird feeling,” explained Dr. Kalman. “If I didn’t grow up in this environment, I think my perspective would be very different.”
And while the DOCS program helps break down the expense barrier, Dr. Kalman notes that the financial burden is more complex, highlighting a spectrum of coverage – ranging from insurance to Ontario Works coverage to none at all. This can complicate who is able to receive what care, where and when.
Embarrassment about lack of oral health care, a misconception of dentistry as painful, or a past traumatizing dentistry experience can also deter people from seeing a dentist.
“We don’t judge when we see patients. We tell them what the problem is and potential solutions,” said Dr. Kalman. “Going into the community and meeting them is a critical component, now it’s less intimidating when you bring them here into the clinic.”
But a sometimes overlooked barrier is simply that medically, the issues patients are experiencing coming into the clinic are becoming more complex, with Dr. Kalman saying a higher percentage of patients need to be referred out to specialists.
Dr. Kalman also places an emphasis on equipping students with the tools they need to work with marginalized populations, who may be experiencing other mental or physical health problems that can make working with them in a dental clinic more challenging.
“When you look at marginalized populations and social determinants of health, mental health is a big one,” Dr. Kalman explained.
But to ensure more individuals are understanding the essential link between oral health and overall health, and accessing the quality care they need, Dr. Kalman says community programs are a “vitally important” part of the equation.
“Collaboration is key. Without the dentists, hygienists, volunteers and community partners we wouldn’t have this,” said Dr. Kalman. “I’m just a guy with a passion, but you need that team.”
DOCSKids
An offshoot of the well-established DOCS, the DOCSKids program sees dental students partnering with libraries, community and family resource centres and schools to teach children about oral health.
“It’s great to be able to serve the community and provide children with access to information and resources they might not otherwise have,” said Caitlin Loo, Dentistry Class of 2022 and one of the student program coordinators of DOCSKids. “It’s rewarding to give back. We’re able to use the knowledge and training we’ve gained in a way that benefits people and makes a real impact.”
Made up of a team of around 100 volunteer dentistry students, the program hosts sessions throughout London during the school year. They provide toothbrushes and toothpaste to the children, but the focus is on education, like teaching kids how to properly brush and floss. “We want to teach kids how to take care of their teeth early on – it’s better to prevent problems,” said Loo. “It sets a foundation for the rest of their life.”
“We want to teach kids how to take care of their teeth early on – it’s better to prevent problems,” said Loo. “It sets a foundation for the rest of their life.”
The team uses interactive games – like matching sugar jars to common foods – to keep kids engaged in their learning. Parents who attend the program are also provided with educational resources.
“A lot of parents and families might not have dental insurance, or some might not have seen a dentist for a few years, so the information we are giving them is quite critical,” said Loo.
This teaching, Loo says, helps in the development of her and her fellow classmates’ communication skills as well, learning how to explain important dental concepts in simple ways.
But a big priority for the program is to expose children to dentists while they are young to help them feel more comfortable at future visits.
“Fear and anxiety about going to the dentist can be a major barrier that prevents people from accessing dental care,” Loo explained. “By having children interact with the dental students doing fun activities in a familiar setting, we’re hopefully teaching them that they don’t need to be afraid of dentists and that taking care of their oral health can be a positive experience.”
Oral Cavity Cancer Screening Program
 At the Salvation Army in London, Ontario, Dr. Hannah Ernst, a third-year resident in Otolaryngology-Head and Neck Surgery, has set up an oral cavity cancer screening program. She’s working alongside Otolaryngology-Head and Neck Surgery faculty member Dr. Danielle Macneil, as well as oral maxillofacial surgeon and Dentistry faculty Dr. Henry Lapointe.
At the Salvation Army in London, Ontario, Dr. Hannah Ernst, a third-year resident in Otolaryngology-Head and Neck Surgery, has set up an oral cavity cancer screening program. She’s working alongside Otolaryngology-Head and Neck Surgery faculty member Dr. Danielle Macneil, as well as oral maxillofacial surgeon and Dentistry faculty Dr. Henry Lapointe.
An aspiring global surgeon, Dr. Ernst sets up a screening station during the Sunday night community meal, where alongside other practitioners, she provides a basic oral cavity inspection and dentition inspection to upward of 40 people per night. With the help of Dr. Lapointe, the program also attempts to address simple and modifiable oral health concerns with oral surgery assessments and referrals.
“This program was born out of a desire to give marginalized and homeless populations a positive healthcare experience,” said Dr. Ernst. “From all my years working with them on the street, they don’t like coming to the hospital or clinic, and they only come when they absolutely need it.”
Participants also fill out a questionnaire regarding their health and oral cavity cancer risk factors and are educated on oral health best practices. The objective of the program is to not only screen but to provide education and prevent oral concerns from developing.
Dr. Ernst says community outreach plays a major role in breaking down multiple barriers to quality health care. First, the resident acknowledges that something seemingly as simple as transportation can be an issue for homeless populations, who may not even have the means to take the bus to a hospital. She also cites mental health barriers or issues managing scheduling and appointments as barriers to traditional health care.
First, the resident acknowledges that something seemingly as simple as transportation can be an issue for homeless populations, who may not even have the means to take the bus to a hospital. She also cites mental health barriers or issues managing scheduling and appointments as barriers to traditional health care.
“I think it’s super important to try to meet people where they are at,” explained Dr. Ernst. “It recognizes that people have huge barriers to health care, and it’s not always that they don’t want to come, sometimes they cannot.”
She also says getting into the community and connecting with people one-on-one helps humanize doctors to marginalized populations, who can sometimes have negative perceptions about the health care system.
“The point is to reach out into the community, connect with people, acknowledge their barriers and help them overcome them so we can work together,” said Dr. Ernst.