Making complex chronic diseases a little less complex
 Complex chronic diseases represent a major threat to Canada’s health care system and to Canadians’ quality of life. Researchers are working with new technologies to better understand the molecular profiles of these diseases and inform new therapies.
Complex chronic diseases represent a major threat to Canada’s health care system and to Canadians’ quality of life. Researchers are working with new technologies to better understand the molecular profiles of these diseases and inform new therapies.
By Sharon Oosthoek, HBA’88
Roughly 44 per cent of Canadians are dealing with at least one complex chronic disease, most of which have no cure and lack adequate treatment.
Whether it is osteoarthritis, inflammatory bowel disease, cancer or cardiovascular disease, the burden “has done nothing but increase decade over decade,” said Dr. Tom Appleton, PhD’07, MD’11, Professor, Medicine and Chief, Rheumatology at St. Joseph’s Health Care London. “Most live with more than one complex chronic disease – as obesity increases, for example, so do things like heart disease and joint disease.”

“To have this full suite of capabilities is really exciting. We are bringing this equipment to all areas of discovery research. In fact, we’re looking at potentially being a service centre for all of Canada.” — Dr. Tom Appleton
Partly the result of longer lifespans, these diseases represent the greatest threat to our health care system and to Canadians’ quality of life. “It’s far outpacing our ability to provide the best care possible for everyone,” said Appleton. He is the principle investigator in a new molecular profiling project at Schulich Medicine & Dentistry that aims to discover more efficient and targeted treatments.
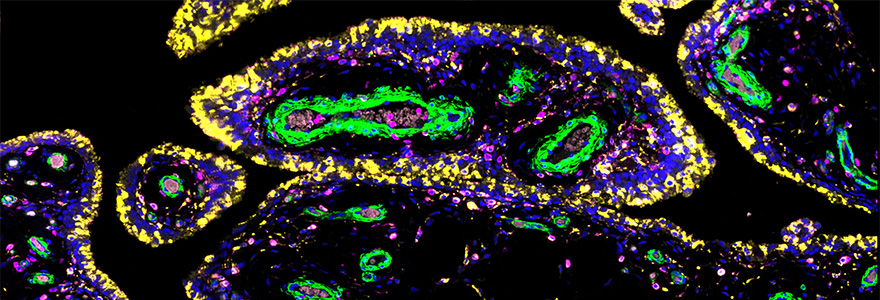
Traditional molecular profiling technologies allow researchers to peer deep into individual cells to identify disease-causing genetic mutations. While this is important information, it comes at a cost. Tissue samples must be broken up in order to isolate and study a given cell. This means it’s no longer possible to know what cells are located next to each other – whether they are part of a tumour, heart muscle or joint.

“We want to know how to manipulate stem cells to enhance their regenerative capacity. If we can see stem cells in situ, we can know better how to promote their work when there is injury and stop the signals that hobble them.”
— Dr. Samuel Asfaha
Knowing where a cell is in relation to other cells is important. “Some cells act to cause disease while others are recruited to fight disease. Up until now, we haven’t been able to tell them apart,” said Appleton. “We want to be able to treat cells driving disease without harming cells that are coming to help.”
Thanks to funding through the Canada Foundation for Innovation, Appleton and his team are a step closer to this kind of precision medicine. In the coming months, he and his co-investigator, Dr. Geoffrey Pickering, PhD’90, Professor, Medicine, will take delivery of a digital spatial profiler.
It will allow London-area biomedical researchers to study the behaviour of individual cells within an intact tissue sample. The profiler may not look like much – it’s about the size and shape of a kitchen microwave oven – but the microscopic pictures it produces will, for the first time, offer a map of what cells are doing and where they are doing it.
Appleton likens it to zooming in on different areas of Canada – it’s one country, but the way winter affects London, Ontario could be very different from the way winter affects Victoria, British Columbia. “It’s the same thing when looking at how tissues are affected by osteoarthritis. One region might be affected differently than another,” he said.
According to gastroenterologist Dr. Samuel Asfaha, Associate Professor, Medicine, who is involved in the project, just one or two companies have developed the technology to do this. “Most institutions don’t have this. There are maybe a handful in Canada,” he said.
 Dr. Geoffrey Pickering
Dr. Geoffrey Pickering
Asfaha is eager to use the profiler to nail down the cellular origin of colorectal cancer and better understand how the gut repairs itself in inflammatory bowel diseases (IBD). Since IBD can be a precursor to colorectal cancer, he is focused on getting a better handle on how the gut’s stem cells replace injured cells, and normally stave off progression to cancer.
“We want to know how to manipulate stem cells to enhance their regenerative capacity,” said Asfaha. “If we can see stem cells in situ, we can know better how to promote their work when there is injury and stop the signals that hobble them.”
For example, a mutated gene in one cell might produce a protein that triggers change in neighbouring stem cells, but not in stem cells further removed. “One cell that’s right next to a stem cell might be secreting something that’s very important to that stem cell’s function. The technology to show us that simply didn’t exist before,” he explained.
“To have this full suite of capabilities is really exciting,” added Appleton. “We are bringing this equipment to all areas of discovery research. In fact, we’re looking at potentially being a service centre for all of Canada.”








