Caring for our defenders
 Schulich Medicine & Dentistry is home to ground-breaking research in military medicine
Schulich Medicine & Dentistry is home to ground-breaking research in military medicine
By Pat Morden, BA’75
Improving care on the battlefield
Dr. Rich Hilsden, who has been a member of the Canadian Armed Forces for nearly 20 years, deployed twice as a surgeon, once to Iraq and once to West Africa. What he saw changed his career trajectory.
“I realized I wanted to play a bigger role in the battlefield medicine system,” he said. “When you’re doing trauma care on the battlefield, every case is life and death.”
He returned to Canada and trained to become a trauma surgeon.
Today, Hilsden is part of a significant military medicine group in London with a close association to Schulich Medicine & Dentistry. “This is one of the best places in the country to be a military doctor,” he said. In addition to those like himself who are full- or part-time members of the Armed Forces, several faculty participate in research on militaryrelated topics.
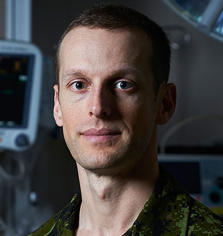
“This is one of the best places in the country to be a military doctor.”
— Dr. Rich Hilsden
Hilsden and his colleague, Dr. Shane Smith, both Assistant Professors at Schulich Medicine & Dentistry, have focused much of their research on preventing hemorrhage, a critical part of trauma care on the battlefield. They have explored the effectiveness of junctional tourniquets to block blood flow from groin injuries. Junctional tourniquets can be applied by trained medical technicians with no special equipment and may help buy time while a soldier is transported to a surgical centre.

“I can count on humanity to create conflict, and while I find that absolutely abhorrent, I do think there’s a responsibility to have a confident and capable medical response to injuries that occur in a military environment.” — Dr. Curtis Van Doormaal
They have also investigated the use of Resuscitative Balloon Occlusion of the Aorta (REBOA). REBOA involves inserting a catheter through the groin area into the aorta and then inflating a balloon to stop bleeding below that point. A more complex procedure, it must be performed by a doctor. Other interests include understanding the best forms of vascular access in far forward positions and the use of whole blood for battlefield transfusions.
Enhancing training and tools
Dr. Curtis Van Doormaal walked into a recruitment office as soon as he was accepted into medical school in 2008. After serving as a family doctor for military personnel in Southern Ontario and deploying as a flight surgeon in Kuwait, he completed additional training as an anesthesiologist. The resident alumnus now works in the Level 1 trauma unit at London Health Sciences Centre and as an emergency doctor in community hospitals.
“It’s a good mix of working in an environment where I have all the people and equipment and blood products I need, and working in a community environment where resources are more limited, more like being deployed.”
As a medical student, Van Doormaal developed a simulation using pork ribs to train the insertion of chest tubes. Since then, he has planned and participated in a variety of realistic simulations based on challenging trauma cases. Participants learn how to communicate effectively in stressful situations, and to practise the critical skill of crisis resource management, the ability to set priorities and delegate in a situation where there are more tasks than time.
Van Doormaal’s research includes exploring applications of point-of-care ultrasound to diagnose on the battlefield, and E-FAST, the use of ultrasound to detect fluid in the chest cavity. He is also developing advanced techniques for acute trauma pain management using ultrasound guidance and regional nerve blocks.

Going forward, he hopes to play a role in developing blood products that have a longer shelf life at room temperature.
Healing invisible wounds
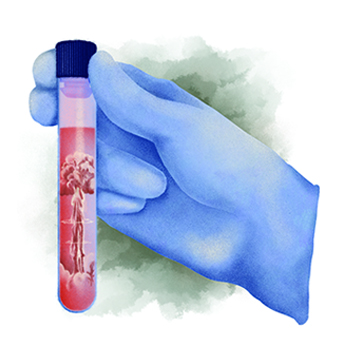
The kind of injuries that Dr. Douglas Fraser, Professor, is studying don’t bleed. They are the invisible injuries caused by repetitive low-level blasts, such as those produced by artillery, mortars, and even by large-calibre weapons used by snipers.
“Soldiers with repetitive exposure over short time periods or over years start to have symptoms that look very much like concussion,” said Fraser. “They report poorer health and quality of life.”

“Soldiers with repetitive exposure over short time periods or over years start to have symptoms that look very much like concussion. They report poorer health and quality of life.” — Dr. Douglas Fraser
Because he has a long-standing interest in the treatment of concussion, Fraser was approached by scientists from Defence Research and Development Canada to help them explore this problem.
Fraser and his collaborators analyzed blood samples from soldiers exposed to blasts, as well as a control group, and conducted a battery of clinical and psychological measures.
They found a set of metabolites that had changed more in the subjects exposed to repetitive blasts. Some were volatile organic compounds, which are released from the body in breath, raising the possibility that a ‘breathalyzer’ could be used as a health surveillance tool.
The study also pointed to the possibility of dietary supplements to cause the metabolites to normalize. A clinical trial is now underway to validate the use of breath to identify blast injury.
Understanding the effects of trauma on the brain
Dr. Ruth Lanius, Professor, also deals with a type of injury that is invisible – post-traumatic stress disorder (PTSD). Her research brings together clinical expertise as a psychiatrist with a longstanding interest in neuroscience.
 One stream of research seeks to understand what happens to the sense of self and identity after trauma. Lanius and her colleagues have identified a critical brain network that may be responsible.
One stream of research seeks to understand what happens to the sense of self and identity after trauma. Lanius and her colleagues have identified a critical brain network that may be responsible.
“When someone is not traumatized, the network is very well connected, and that helps you have a sense of past and future and an embodied sense of self in space,” she said. “When the network is disrupted after trauma, it may be related to a sense that ‘I’m not me anymore.’”
On the other hand, when PTSD patients are under conditions of hyper-arousal, the network may become somewhat connected. This may lead them to reckless behaviour to recover a sense of self.

“When the network is disrupted by trauma, it may be related to a sense that ‘I’m not me anymore.’” — Dr. Ruth Lanius
Lanius is exploring innovative therapies including neurofeedback and deep brain reorienting. Deep brain reorienting is based on the idea that the first response to a stressor is to turn the head toward the threat. The therapy involves bringing up a traumatic memory and encouraging the patient to focus on tension in the shoulders, neck and head as it peaks and then resolves. As the therapy continues, the patient learns to recognize that the emotion they feel is experienced in the body.
In another study, Lanius and her collaborators are exploring what happens in the brain when a soldier recalls a moral injury – something that the person feels they have done wrong or failed to do. The researchers have identified the posterior insula, a part of the brain associated with both visceral sensations in the body and with moral disgust, as an area more activated in people with PTSD.
“Participants tell us that it feels like something’s eating them up inside,” said Lanius. “We’re working to target those visceral sensations. Usually, as they resolve we also see that the negative thoughts start to resolve too.”

A commitment to service
Hilsden believes it’s important to provide high-quality military medicine for two reasons. “We are what is called a ‘force multiplier,’” he said. “Knowing that there’s a surgeon nearby creates a degree of boldness, certainty, and strong morale in the fighters.”
Just as important, of course, is the imperative to provide good care to young women and men who are risking their lives for the country.
“I can count on humanity to create conflict, and while I find that absolutely abhorrent, I do think there’s a responsibility to have a confident and capable medical response to injuries that occur in a military environment,” said Van Doormaal.








