Navigating Uncharted Territory
Dr. Ian Ball has emerged as an influential voice at the intersection of organ donation and medical assistance in dying
By Ashley Rabinovitch
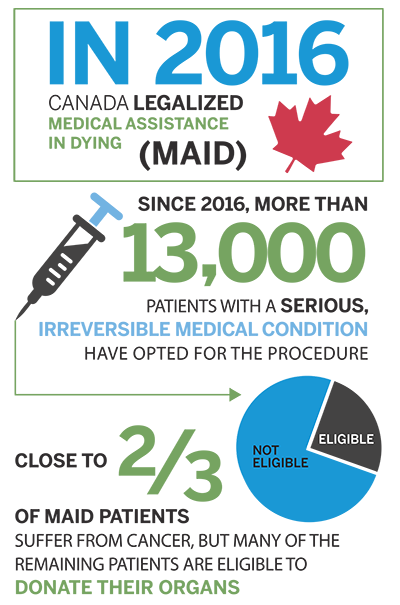
In the four years that have passed since Canada legalized medical assistance in dying (MAID), more than 13,000 patients with a serious, irreversible medical condition have opted for the procedure. Many are eligible to donate their organs, a possibility that has sparked an ongoing ethical debate within the medical community. As one of Canada’s leading experts in organ donation after MAID, Dr. Ian Ball finds himself at the centre of the conversation.
 “I didn’t feel strongly for or against MAID back in 2016,” said Dr. Ball, an Associate Professor in Medicine and Epidemiology and Biostatistics.
“I didn’t feel strongly for or against MAID back in 2016,” said Dr. Ball, an Associate Professor in Medicine and Epidemiology and Biostatistics.
Months before MAID legislation took effect, Dr. Ball joined a group of colleagues at London Health Sciences Centre to talk through its implications.
“That meeting was a turning point for me,” he reflected. “It became evident that there were very few doctors willing to take on MAID cases, so I added my name to the list. Given my experience as an ICU physician, I had a comfort level with anaesthetics and experience with the withdrawal of life support.”
Dr. Ball assessed and performed the first MAID case in London only six weeks later.
“It’s been incredible to witness the comfort it gives MAID patients to have control with their deaths,” he said. “They no longer have to fear unacceptable levels of pain and deterioration.”
Close to two thirds of MAID patients suffer from cancer, but many of the remaining patients are eligible to donate their organs. If anyone can grasp the complexity of pairing MAID cases with organ donation, it’s Dr. Ball. In 2014, he joined the faculty to develop research programs in rehabilitation for the critically ill, organ donation and end of life care.
“Both MAID and organ donation are incredibly complicated by themselves, so pairing them is akin to a space shuttle launch,” he said. “It requires a significant amount of planning and collaboration between Trillium Gift of Life Network, the hospital MAID program and the operating room.”
“Both MAID and organ donation are incredibly complicated by themselves, so pairing them is akin to a space shuttle launch. ” — Dr. Ian Ball
According to Dr. Ball, physicians who transfer organs for transplant have abided by the ‘dead donor rule’ for more than 40 years. “This rule stipulates that the cause of death cannot be organ donation,” he explained. For donations made after cardiocirculatory deaths (DCD), physicians remove life support and wait five minutes before removing the organs to make sure the heart does not restart by itself.
In 2018, Dr. Ball co-authored a paper in the New England Journal of Medicine that questions the validity of the dead donor rule for MAID cases.
“Every MAID patient receives a highly lethal dose of medicine, so the chances of their heart spontaneously restarting are essentially zero,” he wrote.
His paper also raised the possibility of removing organs even before the patient’s heart has stopped to transfer them in the best possible condition.
 “The paper provoked a flood of responses, both positive and negative, but we weren’t picking a side,” Dr. Ball emphasized. “We simply raised the point that organ donation protocol was developed before MAID, and it’s time to reevaluate whether or not MAID organ donation merits its own pathways.”
“The paper provoked a flood of responses, both positive and negative, but we weren’t picking a side,” Dr. Ball emphasized. “We simply raised the point that organ donation protocol was developed before MAID, and it’s time to reevaluate whether or not MAID organ donation merits its own pathways.”
According to Dr. Ball, members of the Canadian public typically have more relaxed views on organ donation than doctors and policymakers realize.
For a research paper published in the Canadian Journal of Anesthesia in 2020, he and his colleagues surveyed 1,000 Canadians to gauge support for a procedure that entails restarting the heart after the patient’s death before transplanting it. More than eight out of ten respondents were supportive, the survey found.
“Our experience and preliminary research results indicate that most members of the public are more concerned with issues of patient comfort and autonomy than the medical and surgical details of organ donation,” noted Dr. Ball.
Despite high levels of public support for MAID, organ donation, and the combination of the two, only 30 MAID patients in Ontario have donated their organs.
“Whenever I give public talks, it surprises me how many people still don’t know that MAID is an option,” said Dr. Ball.
Every three days in Canada, a person who is on the waiting list for an organ dies. While only a minority of MAID patients are eligible to donate their organs, improving awareness among those who are eligible can help save lives.
“I’ve seen what an enormous relief it brings to the families of donors to realize that their loved ones have saved up to eight other lives through organ donation,” he affirmed.
For several months in early 2020, Dr. Ball and his colleagues were forced to put the MAID program on hold to respond to the COVID-19 pandemic. They have slowly started to accept new MAID cases and resume their research efforts. “As we continue researching MAID and organ donation, we’ve also initiated a project to gather more national data on MAID programs so that we can learn from what others are doing to improve patient care. There is still a lot of work to be done.”








