Creative Collaboration
A unique school granting program is funding out-of-the-box research projects for interdisciplinary teams from across basic and clinical sciences
By Jesica Hurst, BA’14
What would happen if physicians helped critically ill patients exercise while they were still receiving treatment in the intensive care unit (ICU) of a hospital?
It’s a question that had not been well studied before a group of researchers at Schulich Medicine & Dentistry came up with the novel idea.
For the past century, the typical clinical approach has been to let critically ill patients rest, as physicians did not want to harm them or put them at higher risk.
Studies have shown that exercise is beneficial to the recovery of these patients after they are awake and able to take part in physical activity themselves, but no one had ever attempted to study the effects of helping these patients exercise sooner.
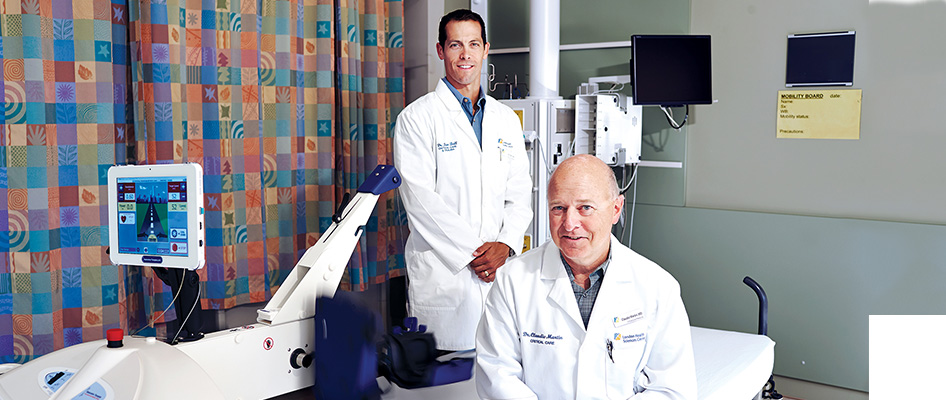
Drs. Doug Fraser and Claudio Martin and Kevin Shoemaker, PhD, came together in 2012 to discuss the possibility of challenging the typical approach. They wanted to look at the effects of targeted passive exercise on patients with sepsis—a potentially life-threatening complication that occurs after a severe infection.
Their plan was to utilize passive cycle ergometers, which are motorized cycling machines that patients can be hooked up to while resting or under medically-induced comas.
 “We all asked the question, why do we have to wait until the patient has been released from the ICU to start the process of exercise and rehabilitation?’’ Dr. Martin said. “We got excited about the idea of pushing the limit and testing our theory that having patients exercise sooner could potentially help their recovery process.”
“We all asked the question, why do we have to wait until the patient has been released from the ICU to start the process of exercise and rehabilitation?’’ Dr. Martin said. “We got excited about the idea of pushing the limit and testing our theory that having patients exercise sooner could potentially help their recovery process.”
“Many of these patients can’t move, because they are immobile or have severely damaged muscle and/or cognitive abilities,” Shoemaker added. “The idea was to simply induce passive exercise at an earlier stage, have the machine do all of the work for the patients, and to study the outcomes on the blood vessels.”
Shortly after the three researchers met, they developed a large interdisciplinary team of basic scientists and clinician researchers to work together on the project, which is comprised of Dr. Ian Ball; Gedas Cepinskas, PhD; Chris Ellis, PhD; Dr. Fraser; Keith St. Lawrence, PhD; Dr. Martin.
“We got excited about the idea of pushing the limit and testing our theory that having patients exercise sooner could potentially help their recovery process.” — Dr. Claudio Martin
Dr. Tina Mele and Shoemaker. They come from a variety of departments, including Medical Biophysics, Medicine, Pathology and Laboratory Medicine, Surgery, Anesthesia & Perioperative Medicine, Paediatrics and the Faculty of Health Sciences.
The group applied for Schulich Medicine & Dentistry’s Collaborative Research Seed Grant (CRSG) competition’s first round, and received the funding they needed to move forward with their innovative project, which included recruiting 10 patients for their clinical study.
When Dr. Ball was recruited from Queen’s University by Dr. Martin to help lead the clinical portion of the study and manage the day-to-day activities of the group, he was incredibly excited. Known as ‘the exercise guy’ by colleagues, he never thought he would be able to blend his professional work with his passion for exercise, health and fitness.
“Patients in the ICU spend a lot of time lying in bed, so to feel that they were able to do something that could actually contribute to their improvement was very appealing to them.” —Dr. Ian Ball
Dr. Ball helped recruit the patients they needed to complete the clinical portion of their research.
“It was interesting how families and patients themselves were really excited about the idea of participating in this novel study,” Dr. Ball said. “Patients in the ICU spend a lot of time lying in bed, so to feel that they were able to do something that could actually contribute to their improvement was very appealing to them.”
The first step of the clinical portion of the study is now complete, and the next step is for Dr. Fraser, Cepinskas and Ellis to analyze the findings. This will help them determine how to move forward with the research.
“Before and after the patients took part in the passive exercise, we took blood from them to analyze,” Dr. Fraser said. “Gedas and I are currently working together to look at various biomarkers of inflammation that could help determine whether or not there is any indication that there is a positive effect.”
“When it comes to large externally-funded grants, there really is no place to take risks because granting agencies want to ensure researchers can deliver positive findings.” —Denise Figlewicz, PhD
Ellis had been working with Martin and his team for years on projects related to sepsis and inflammation, but never considered passive exercise as a potential therapy for critical care patients. Like Dr. Ball, the idea made him excited and intrigued.
Ellis and his lab members developed what they consider a ‘replica ICU’ for animal models—a place where they could mimic what the clinician-researchers would be studying in the hospitals.
“I thought it would be neat to reproduce the clinical work they were doing in our lab by reproducing the same type of disease of sepsis in our animal models, and reproducing passive exercise to study its effect,” Ellis explained. He added that it is important to include the basic science aspect of the research because they can study the animal models in much more depth and detail than the clinicians could study the human patients in the ICU.
Denise Figlewicz, PhD, vice dean, Research & Innovation, explained that the idea of launching the CRSG competition came from conversations about how to fulfil the objectives of the School’s strategic plan.
“In the strategic plan, there is a mandate to do several things including strengthening knowledge translation, promoting an interdisciplinary research environment, and fostering interactions between researchers and knowledge users through the formation of teams,” Figlewicz said. “Many new funding opportunities with large awards require multidisciplinary teams to tackle the complex problems involving the development of new care approaches, therapies or methods of care delivery. Thus, in creating the CRSG program, we are responding to both internal and external mandates.”
Figlewicz added that the most exciting part of this internal funding competition is the fact that the projects most likely will be high risk—they want researchers to bring novel ideas forward, acknowledging that their hypotheses could potentially be wrong.
 “When it comes to large externally-funded grants, there really is no place to take risks because granting agencies want to ensure researchers can deliver positive findings,” she explained. “While that does make sense, what happens is the cool ‘lightbulb’ ideas never get their chance, and that is sometimes where the real research magic happens.”
“When it comes to large externally-funded grants, there really is no place to take risks because granting agencies want to ensure researchers can deliver positive findings,” she explained. “While that does make sense, what happens is the cool ‘lightbulb’ ideas never get their chance, and that is sometimes where the real research magic happens.”
Since its launch in 2013, the Research Office has received at least 25 applications per year. The Office has funded 20 innovative projects to date.
Dr. Mele said the opportunity to work on a project with both clinician researchers and basic scientists is not only exciting and more rewarding, but it can also lead to more meaningful results.
“A lot of what we do in the ICU is supportive care, but by changing the focus to the cellular mechanisms of what is going on in patients, we could potentially improve their mortality,” Dr. Mele said. “Bringing two groups of researchers together who have two different perspectives could potentially help us solve this problem.”
Shoemaker agreed, adding that a collaborative approach to research problems like this one can identify results that can help patients sooner.
“If exercise is going to be implemented as a treatment, there is still so much that we need to know,” Shoemaker said. “In order to find those answers we need to work as a team—we need a lot of people and their expertise, and we need these funding opportunities to further the work we have started.”