Bringing Infection to its Knees
A team of researchers is working to reduce infection rates for millions of people who undergo orthopaedic surgery
By Debora Van Brenk, BA’86, MA’87
Despite a host of medical, biological and engineering milestones in orthopaedics and musculoskeletal research, infection rates in orthopaedic surgery haven’t moved significantly in decades.
But clinicians and researchers at Schulich Medicine & Dentistry are at the forefront in working to move that needle for millions of people who have experienced bone trauma or had joint replacements. “Infection prevention, detection, diagnosis and treatment have been identified globally as the major issues in the orthopaedic field, and a top priority for musculoskeletal research,” said Dr. Emil Schemitsch, Chair/Chief, Surgery.
“This is an absolutely critical problem. It is largely unsolved and it has a huge impact on patients and society,” he added.
Infection rates after trauma surgery can run as high as 40 per cent. And after some types of joint replacements, one in 50 patients may get a serious infection, leading to poor outcomes, reoperation and residual long-term disability. The infection rate is even higher in patients with comor-bidities or a history of previous surgery.
David O’Gorman, PhD, a Professor of Biochemistry and Surgery, is part of a team of researchers tackling the problem from all angles.
“After shoulder joint replacement, for example, an infection may quietly eat away at connective tissue for a month or more before it is detected clinically,” O’Gorman said.
And while the incidence of this infection is relatively low – between two and three per cent of patients – it typically results in the need for an additional surgery to remove the implant, added time to treat the infection and then a third surgery to implant a second artificial shoulder joint.
In addition to the huge toll this takes on a patient’s physical and mental health and their families, the complication is expensive: costing three-to-13 times more than the original joint-replacement procedure.
O’Gorman, who is also a scientist at Lawson Health Research Institute, is currently focused on a problematic bacteria called Cutibacterium acnes, which have a particular affinity for artificial shoulder joints.
“Imagine putting on the hat of a surgeon and being able to say to a patient, this used to be a problem and patients like you sometimes had serious complications. But not anymore. We’ve managed to get this under control.” — David Holdsworth, PhD
Believed to originate in the sebaceous glands of the skin, Cutibacterium acnes make their way into the dark, warm and oxygen-depleted (anaerobic) recesses of the new joint and hide there. Then they multiply and eat connective tissue such as muscles, tendons and ligaments.
Once the infection has been “cooking away for a couple of weeks,” the implant can become loose or too painful and needs to be removed and replaced. “This particular microorganism is sneaky. It has methods for avoiding immune-system detection we still don’t understand,” O’Gorman said.
One obstacle to detection and treatment is the “goop” (biofilm) that the bacteria secrete around themselves, a layer that both hides them from the body’s immune response and defies the effectiveness of antibiotics.
O’Gorman’s lab is combining artificial human tissues, implant metals and Cutibacterium acnes cultures to replicate this infection process in the lab. They aim to understand the mechanisms that these bacteria use to “eat” joint tissues, and ways to dissolve that goopy biofilm to make the infection discoverable to the immune system and to antibiotics. They are also searching for new biomarkers secreted either by the bacteria or by the infected tissues to help detect and treat these infections before they do too much damage.
David Holdsworth, a Professor in Medical Biophysics and the Scientific Director at Western’s Bone & Joint Institute is another member of the research team and is excited about the prospect of improving patients’ odds.
“It would be wonderful if we never had to do these surgeries more than once,” he said.
“Imagine putting on the hat of a surgeon and being able to say to a patient, this used to be a problem and patients like you sometimes had serious complications. But not anymore. We’ve managed to get this under control.”
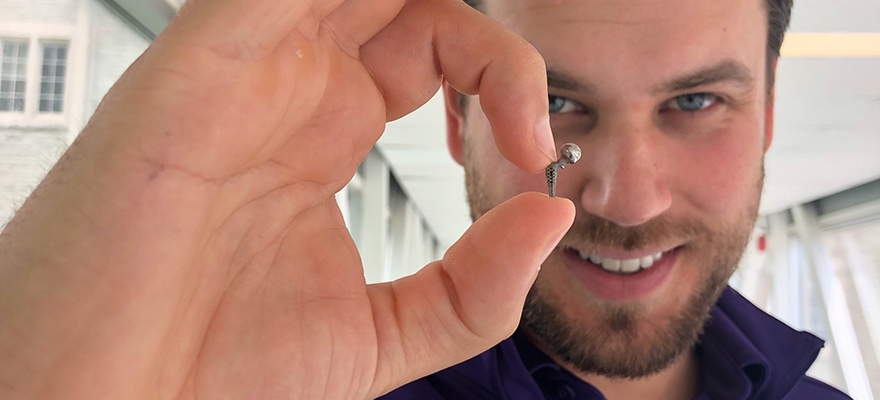
Holdsworth, who is also a scientist at Robarts Research Institute, has reapplied some of his research to tackle the problem more directly. Imaging the interface between bones and metal implants, he has been working to test novel hip implants in rat models, a procedure intended to mimic the human procedure. In addition to studying how the implant fits with bones and the mobility it offers, Holdsworth is now working to understand patterns of infection and infection recovery among these models.
Brainstorming among the group has led to some novel hypotheses for processes and treatments that could detect and kill lurking bacteria.
“We all play roles in this and it’s a big team,” Holdsworth said.
For his part, Dr. Schemitsch is tackling the issue through surgical processes and procedures.
As a surgeon who implants many new hips and knees into patients younger than 65, Dr. Schemitsch says it’s in everyone’s best interest to ensure the implants have longevity.
Improved surgical approaches, better antibiotics, improved sterilization protocols, more robust devices and better understanding of anatomy have all led to important advances in orthopaedics practice and better patient outcomes, he said.
“Despite that, we still haven’t put a significant dent in infection rates in patients with implants,” he noted.
And in people who have had orthopaedic trauma – such as an open fracture of the tibia – those infection rates can be as high as 40 per cent.
An infection for these patients can have life-altering consequences as well as major social and societal impact. “We’re looking at a number of things both in patients and in the lab to improve the odds,” Dr. Schemitsch said.
For Dr. Schemitsch, a series of effective small steps can prove ultimately to make a big difference.
“Preventing, diagnosing and treatment of infection are all core areas we have to focus on,” he said.
Dr. Schemitsch has concentrated on new implant designs, wound management techniques and surgical process improvements to reduce the burden of infection.
He has been part of a large team that has examined questions about whether washing the wound with soap during surgery, instead of with saline, is more effective (they found saline works better), and whether fluids at high-pressure or low-pressure work better for decontaminating a wound site.
Impregnating calcium sulfate (used to rebuild a bone) with an antibiotic called tobramycin is also effectively preventing infection and prompting faster healing in many patients.
He is working toward better diagnostic tools because determining whether it’s an infection at all can be difficult.
If a patient is in pain, is it part of the healing process, a problem with the implant or is it the start of an infection? And then, if a serious infection has set in, is there an effective way to remove it, treat the infection and salvage/replace an implant in a single surgery, rather than in multiple operations as is often the case now?
If the big questions continue to trouble the scientists, they are equally excited about the opportunities to improve world-wide musculoskeletal care.
“We have a real opportunity to make a huge difference,” Dr. Schemitsch said. “At Western, we’re perfectly situated to make this happen. Orthopaedics and musculoskeletal here are absolutely tops in the country.”
Add to that the local expertise in imaging, immunology, biology, diagnostics, bioengineering, chemistry and clinical work – plus the interdisciplinary power of the Bone and Joint Institute – they hope musculoskeletal infection can be brought to its knees.