Understanding and Treating the ‘Sacred Disease’
Epilepsy is a complicated neurological disorder with no clear answers. Solving the puzzle requires strong, interdisciplinary research – the kind taking place at Robarts Research Institute.
By Emily Leighton, MA’13
Epilepsy was first described in Babylonian texts more than 3,000 years ago. The ancient Greeks called it the ‘sacred disease,’ associating the disorder with the divine. The ancient Romans believed it to be contagious and called sufferers lunaticus, or moonstruck.
During the Middle Ages, it was known as the falling sickness. In many cultures throughout history, people with epilepsy have been stigmatized and isolated due to a lack of knowledge. And in the 21st century, while progress has been made, the mysterious and misunderstood disorder continues to puzzle experts.
A group of scientists at Robarts Research Institute are tackling this challenge, working to improve modern understanding of a long-chronicled disorder and advance promising new treatment options.
Imaging advances: “Surgeons need more information”
As a first line of treatment, epileptic seizures are controlled with medication. But about one-third of people with epilepsy do not respond to drug therapy – in Canada, this means about 60,000 people are living with what’s known as drug-resistant epilepsy.
In this case, individuals may be candidates for a surgery that removes the part of the brain where the seizures originate. But the challenge for surgeons is identifying these precise regions of the brain.
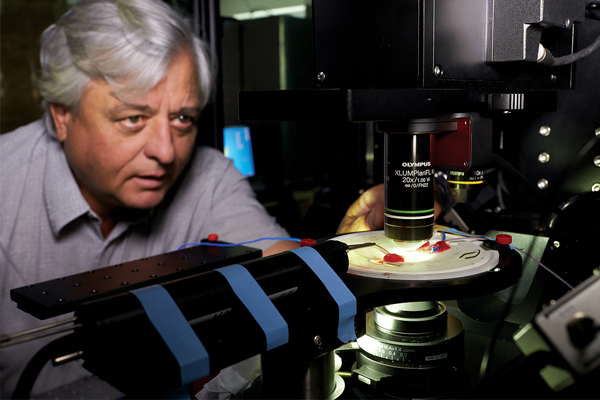
Equipped with advanced imaging technologies, Robarts researchers are developing techniques to improve the accuracy and precision of these surgeries.
“The objective is to find the tissue in the brain that is causing the epileptic seizures and to spare the tissue that isn’t involved. Using imaging technology, we can identify abnormalities in the region that we suspect the epileptic seizures are coming from and look at the networks surrounding that region.” —Terry Peters, PhD
“The objective is to find the tissue in the brain that is causing the epileptic seizures and to spare the tissue that isn’t involved,” said Terry Peters, PhD, who leads the Virtual Augmentation and Simulation for Surgery and Therapy (VASST) Laboratory at Robarts. “Using imaging technology, we can identify abnormalities in the region that we suspect the epileptic seizures are coming from and look at the networks surrounding that region.”
Access to ultra high-field magnetic resonance imaging (MRI) technology at Robarts enables researchers to see the structure and function of the brain that cannot be visualized using standard imaging modalities.
“The pathologies in epilepsy are so subtle, they are basically invisible to conventional techniques,” said Robarts scientist Ali Khan, PhD.
Khan is working with diffusion MRI, a technique that measures how water molecules move around in the brain. During the course of several milliseconds, researchers can detect the motion of water molecules at microscopic scales.
“This gives us a magnifying glass into the structure of the brain,” he explained.
With this microscopic information, he is examining how pathways in the brain are connected, and how they may be disconnected in patients with epilepsy. His team is also interested in how the architecture of the brain’s grey matter differs in epilepsy compared to the general population.
“The research that we’re doing is motivating the precision and accuracy we will need for the next generation of clinical interventions,” said Khan.
“These tools take us from a radiologist looking at greyscale two-dimensional images on a computer screen making somewhat subjective judgements, to quantitative three-dimensional imaging that provides much more valuable information,” added Peters.
 Dr. Jonathan Lau, a neurosurgery resident who is completing a PhD in biomedical engineering with the VASST and Khan Labs, is exploring ways to apply these sophisticated tools in the clinical environment and provide more personalized therapies for epilepsy patients.
Dr. Jonathan Lau, a neurosurgery resident who is completing a PhD in biomedical engineering with the VASST and Khan Labs, is exploring ways to apply these sophisticated tools in the clinical environment and provide more personalized therapies for epilepsy patients.
He is using ultra high-field MRI to more precisely implant depth electrodes in the brains of epilepsy patients (electrodes are used as diagnostic tools to pinpoint the origin of seizure activity in the brain).
“We need to know where to place the electrodes, because we can’t place them everywhere in the brain. We need to be strategic about where they are placed,” he explained. “When we can see where the seizures are coming from, we can target better.”
Dr. Lau says collaboration is essential to shedding light on the disorder. “Epilepsy is a very challenging problem that requires a multidisciplinary team. We need to bring together a lot of people to achieve our goal of more focused and personalized therapy for our patients.”
Understanding the brain: “Epilepsy is complicated”
Robarts scientist Michael Poulter, PhD, has been investigating the neurochemical mechanisms underlying epilepsy for more than 25 years, trying to better understand how the epileptic brain is wired.
“From what we can tell, no two epilepsy cases are identical,” he said. “It’s a very complicated disorder.”
His major focus in recent years has been the connection between stress and epilepsy. “Our goal is to understand why stress causes an increase in seizure frequency and severity,” he explained.
Poulter and his research team have shown that a stress neurotransmitter called corticotropin-releasing factor (CRF) changes the activity in the brains of epileptic animal models. In a normal brain, CRF diminishes activity in a region of the brain associated with seizures, but in an epileptic brain, it does the exact opposite – increasing activity.
This research points to new drugs that may prevent stress-induced seizures.
Poulter is also studying traumatic brain injury in relation to epilepsy. Depending on the severity of brain injury, there is an increased chance of developing what is known as “post-traumatic epilepsy.” Studying animal models of traumatic brain injury, Poulter found that applying stress caused the same brain activity that is associated with increased seizures in epilepsy patients.
“This type of epilepsy is probably more common than we realize, since many people get concussions throughout their lives,” he said.
In addition to his scientific work, Poulter serves on the Board of Directors for Epilepsy Canada, a Canadian charity that funds epilepsy research. He says the community keeps him focused and motivated.
“Epilepsy can greatly impact a person’s quality of life. People with uncontrolled epilepsy may lose out on employment opportunities or suffer from social isolation. We need to be aware of these social and economic issues and continue to push research forward.” —Michael Poulter, PhD
“Epilepsy can greatly impact a person’s quality of life,” he said. “People with uncontrolled epilepsy may lose out on employment opportunities or suffer from social isolation. We need to be aware of these social and economic issues and continue to push research forward.”
Clinical perspectives: “We want answers for our patients”
The epilepsy research taking place at Robarts requires strong clinical partnerships. Robarts’ close proximity to London Health Sciences Centre (LHSC) and national leaders in epilepsy patient care is a major advantage.
“We are extraordinarily lucky to have access to this internationally recognized clinical and surgical expertise,” said Peters.
As Co-Directors of the Epilepsy Program at Schulich Medicine & Dentistry, Drs. Jorge Burneo and David Steven play an important role in this collaborative approach. Their clinical facilities include the 11-bed, in-patient Epilepsy Monitoring Unit (EMU) at LHSC – the largest in Canada.
“We provide guidance for the researchers, to help them ask more meaningful questions and advise if the research will have clinical significance,” said Dr. Burneo, who also co-directs the Ontario Brain Institute’s EpLink program, bringing together researchers, clinicians and community members to improve diagnosis and treatment for drug-resistant epilepsy.
Dr. Steven, a neurosurgeon, has integrated a stereotactic robot into implant surgeries, improving consistency, precision and mechanical accuracy for placing depth electrodes in the brain. Scientists with the VASST Lab at Robarts will soon be acquiring this robotic equipment for research purposes, with the hope of enhancing its capabilities and facilitating more network-based investigations.
“As clinicians, we are involved in research because we want answers for our patients,” said Dr. Burneo. “The research taking place at Robarts is state-of-the-art, and it is helping us provide better care.”