Up close and personal
By Emily Leighton, MA'13
The monster morphs into countless shapes and forms as it lurks within the human body—a mutant intruder that chaotically creeps and multiplies at an alarming rate. Its invasive tentacles forcefully seek new territory, wreaking havoc on the life it so cruelly disrupts.
The monster’s name is cancer.
It is currently estimated that one in four Canadians will succumb to cancer. And the number of new cases is expected to rise by more than 70 per cent during the next 20 years, according to the World Health Organization.
To fight the monster effectively on all fronts, modern cancer research has evolved into a multidisciplinary effort. And innovative forms of imaging are an essential resource.
A team of imaging scientists at Robarts Research Institute is making considerable contributions to this particular quest through the Cancer Imaging Research Program. For them, getting eyes on the disease appears to be a winning battle strategy.
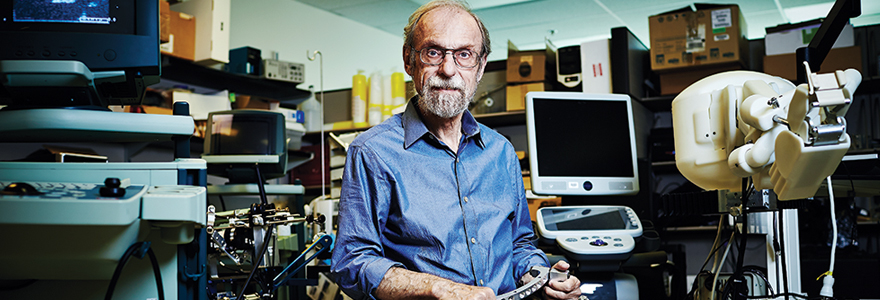
“If you can’t see it, you can’t strike it,” said Aaron Fenster, PhD, director of the Imaging Group at Robarts. “And if you can’t strike it, you can’t cure it.” Fenster is an inventor and scientific whiz. With more than 50 national and international patents to his name, he represents a strong arsenal of knowledge and experience in confronting the cancer monster.
Using 3-D ultrasound, Fenster and his team at Robarts are developing technologies that allow doctors to precisely guide tools for cancer diagnosis and treatment. His lab creates image-guided interventions for breast, cervical, liver and prostate cancers.
“We are looking at diagnosing cancer very precisely and guiding therapies more accurately,” he explained. “The idea is to destroy the cancer through minimally-invasive procedures.”
Fenster’s inventive mind is currently working on an imaging system that will complement cervical cancer treatment. Radioactive seeds are inserted into patients, destroying the cancer from inside. But precision is difficult and potentially inaccurate, as the procedure is currently performed without image guidance.
Using 3-D ultrasound in combination with each patient’s diagnostic magnetic resonance imaging (MRI) scans, Fenster is devising a system that solves this missing visual element. “Physicians will be able to see the procedure as it takes place,” he said.
A bench-to-bedside mentality exists across all of Fenster’s research projects. From inventing solutions for clinical problems to building complete imaging systems, including hardware and software elements, his lab is on the cutting edge of medical imaging and applications.
This remarkable innovation is paralleled by renowned expertise in other imaging fields at Robarts, including research underway by Paula Foster, PhD.
Foster is a scientific detective extraordinaire. Using MRI, she tracks the movement of cancer cells and treatments in the body. The technique, called ‘cell tracking’, is oneof- a-kind in Canada.
Cells are labelled with magnetic nanoparticles, making them detectable with high-resolution MRI. This enables Foster to pinpoint small cellular events in the body that are pre-disease, catching a cancerous lesion or tumour in its earliest phase.
With many of her investigations, Foster tracks breast cancer metastases—secondary tumours that develop in the liver, bone, lung or brain. These particularly vicious manifestations of the disease are responsible for the most breast cancer-related deaths, as the metastatic tumour can be treated but not cured.
An exciting new discovery has also given Foster and her team the ability to detect and monitor dormant cancer cells. Dormancy is a stage in cancer progression where cells do not divide, but survive in an inactive state—the cancer monster quietly waiting to strike again.
“These cells can remain in this dormant state for years, even decades, before waking up, dividing and proliferating to become tumours,” explained Foster. “They exist as ticking time bombs and are believed to be responsible for tumour recurrence.”

"Doctors need to know as early as possible whether cancer treatment is effective or not for their patients." - Ting-Yim Lee
Foster’s lab is working to identify these time bombs before they detonate. “This research has the potential to shed light on one of the least understood aspects of breast cancer recurrence,” she said. “Our studies may lead to the investigation of treatments that target dormant cancer cells.”
Using the same cell labelling technique, Foster is tracking immunotherapy treatment, an experimental therapy that harnesses a patient’s own immune cells to attack cancer. These immune cells are monitored as they migrate throughout the body.
Timothy Scholl, PhD, is also paying close attention to the small details of the disease.
He is looking inside cancer tumours, developing molecular imaging probes to noninvasively assess changes in tumour biology.
These probes are created out of magnetized molecules and subsequently injected as contrast agents, making them visible with MRI as they embark on an explorative mission in the body.
Scholl specifically focuses on tumour metabolism. “If we can see how the metabolism is different in tumours that means we can identify them, determine how aggressive they are and also analyze treatment response,” explained Scholl.

“If we can see how the metabolism is different in tumours
that means we can identify them.” - Timothy Scholl
“Treating a tumour, it might take weeks to notice any difference by conventional methods,” said Scholl. “Working with metabolism allows us to detect change much earlier.”
For Scholl, imaging is a vital tool in confronting the cancer monster. “Imaging allows for the identification of disease and validation of treatment, making cancer care more patient-specific and less costly,” he said.
Visualizing cancer treatment is an important step in realizing this ideal of personalized medicine.
“Doctors need to know as early as possible whether cancer treatment is effective or not for their patients,” said Ting-Yim Lee, PhD. He is using readily available computed tomography (CT) scanners to give physicians this precise ability.
Applying his renowned CT perfusion technology, Lee measures blood flow to and from cancer tumours. Because tumours need blood vessels to survive and grow, they often display an increased number or concentration, known as angiogenesis. CT perfusion indicates if treatment is starving the tumour of these new blood vessels effectively or not.
The goal is to identify which patients will benefit from certain types of cancer treatment, such as angiogenesis-inhibiting drugs, and which will not.
In recent multi-centre clinical trials on cases of liver and ovarian cancer, this technology has proven to be a strong predictor of therapy outcomes. “CT perfusion is a very powerful addition to the monitoring of cancer treatment,” said Lee. “The technology is easily implemented and efficient, and can give physicians a fuller picture of how patients are responding to treatment.”
As is evident by the work underway at Robarts, the power of many exceptional minds is pushing cancer imaging in promising new directions.
With the combined ability to detect the disease at its earliest stages and improved methods of delivering and tracking treatment, imaging research at Robarts is providing hope for the cancer patients of the future.
And with eyes on the disease, these researchers are determined to get up close and personal. Their relentless determination is a warning to the monster; you can run but you can’t hide.