
By Max Martin, MMJC’19
David Heinrichs, PhD, has heard the bleak forecasts.
A November 2019 report, When Antibiotics Fail, by the Council of Canadian Academies, projected a dark future for Canada, where our frontline defence against deadly infections, antibiotics, are weakened, increasing death rates and devastating the country’s economy.
By 2050, 40 per cent of bacterial infections could become antibiotic resistant. If that happens, it’s expected to kill nearly 400,000 Canadians during the next three decades, costing the nation $120 billion in hospital expenses and $388 billion in gross domestic product.
“We’re interested in how we can effectively dismantle the bacteria during infection. We’re finding ways to give the immune system a helping hand.”
– David Heinrichs, PhD
“We are running out of new antibiotics to treat infections,” said Heinrichs, PhD. “That’s where we come in.”
In his lab, the Schulich Medicine & Dentistry Microbiology and Immunology Professor and his team are studying Staphylococcus aureus, commonly known as a Staph A – one of the world’s deadliest bacteria. He’s particularly interested in MRSA, an antibiotic variety of the bacteria often referred to as a superbug.
“Bacteria like this are difficult to treat,” he said. “ S. aureus, like other notable microbial pathogens, can trick the immune system and avoid being killed.”
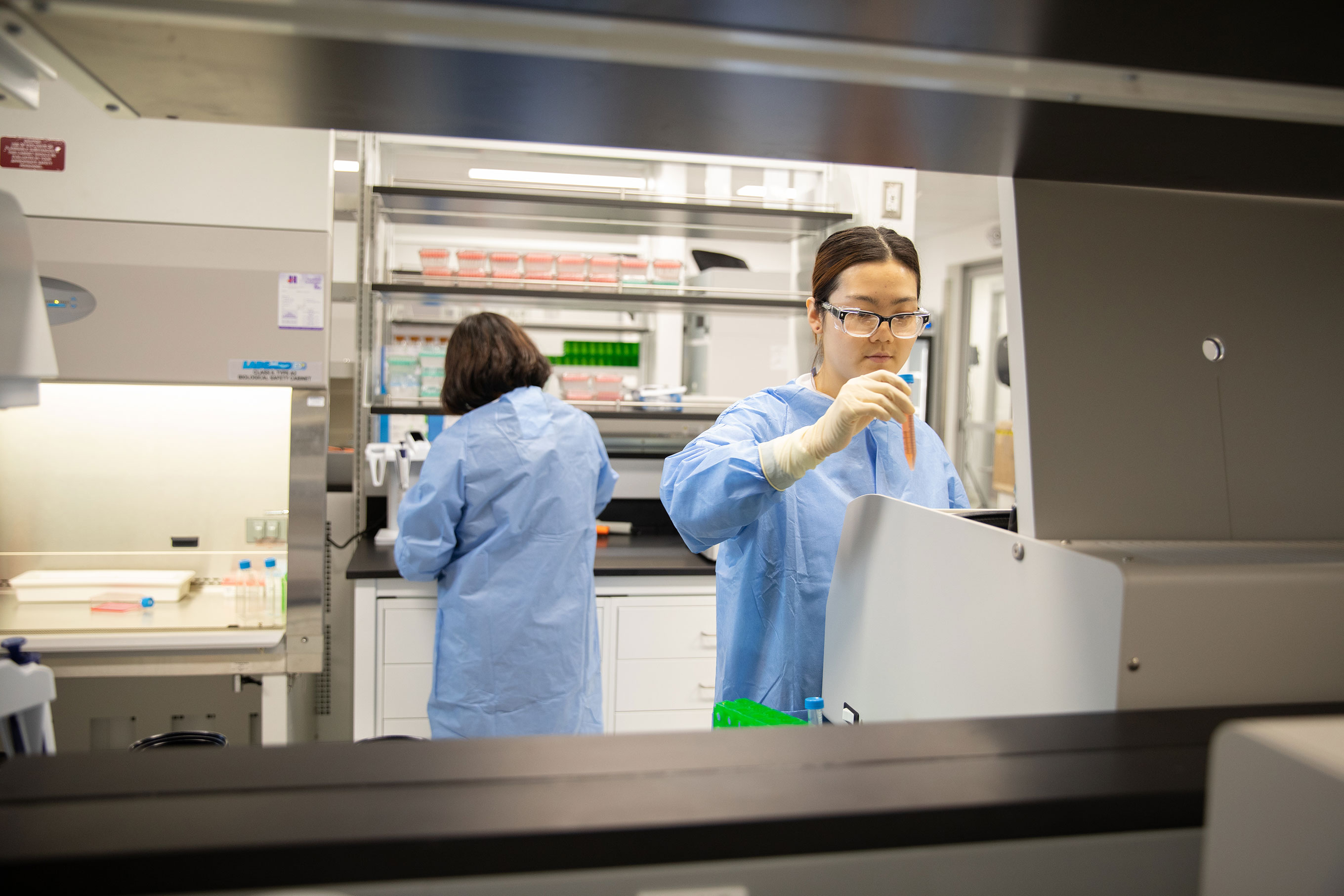
Western’s new Imaging Pathogens for Knowledge Translation (ImPaKT) Facility at Schulich Medicine & Dentistry is setting the stage for Heinrichs’ next wave of research into outsmarting these crafty bacteria.
His ultimate goal is to develop a new antibacterial drug that can work on MRSA.

“We’re interested in how we can effectively dismantle the bacteria during infection,” he said. “We’re finding ways to give the immune system a helping hand.”
And he’s already making significant progress toward dismantling MRSA. Heinrichs was recently involved in a joint study with McMaster University that discovered a potent new antimicrobial that shows promise in fighting staph infections.
The new antimicrobial diminishes MRSA’s tolerance to the immune system and blocks its ability to resist the action of several front-line antibiotics. Since the compound doesn’t kill the superbug directly, the likelihood of antibiotic resistance developing is lessened.
“This molecule can re-sensitize MRSA to be able to be killed by antibiotics,” Heinrichs said. “Our lab showed that this compound also works against Staphylococcus aureus while it resides inside our cells – this is where the bacteria can hide.”
"The ImPaKT Facility will give us access to technologies that will allow us to monitor the entire course of the infection in real time."
– David Heinrichs, PhD
With the imaging suite inside the ImPaKT Facility, Heinrichs can now study MRSA even more closely.
His team will be able to image the bacteria during the course of infection and as it grows inside host cells, providing an even more dynamic visualization of the infection.
“The ImPaKT Facility will give us access to technologies that will allow us to monitor the entire course of the infection in real-time in a living animal model, which is very important,” Heinrichs explained.
They’ll be using bioluminescence imaging equipment, where bacteria are made luminescent, to watch as the infection grows. They’re also able to mark bacteria and immune cells with different dye colours and watch them under powerful microscopes. This will let the team paint an even more detailed picture of infection at the molecular level and study how the infection responds to new molecules that are under development.
All of the equipment is located in ImPaKT’s containment facility, where researchers can safely work with live, infected mice. Heinrichs says this is essential because bacteria grow quite differently in test tubes than they do in living hosts.
Heinrichs and his team will then use various inhibitors at different stages of the infection to see what impact it has on the bacteria. With the new imaging modalities, they’ll also be able to track the bacteria as it spreads throughout the body from organ to organ.
Of particular interest to Heinrichs is the role of macrophages in infection. Macrophages are cells of the immune system that typically eat and then kill bacteria, playing an essential role in curtailing infection in the body.
But when macrophages eat MRSA, it isn’t killed. Instead, the bacteria start to grow inside these cells, eventually bursting out and spreading through the bloodstream and to other organs.
“We’re trying to understand how the bacteria are able to do that. We’ve started to identify some of the genes that are essential for MRSA to survive inside the macrophage. If we knock those genes out, we can actually stop the bacteria from replicating,” Heinrichs explained.
Staphylococcus aureus is found on the skin of nearly 30 per cent of the population, and because humans are exposed to it so frequently, a natural immune response is developed. But MRSA, the super virulent variety of the bacteria that is found on about two per cent of the population, remains untreatable by antibiotics.
It becomes increasingly deadly when bacteria from a skin infection invades deeper into the body and bloodstream, infecting the bones, joints, lungs and heart.
The World Health Organization estimates people with MRSA are 64 per cent more likely to die of their infection than those with treatable strains.
As skin and soft tissue infections are becoming increasingly prominent, especially among athletes and in health care settings, Heinrichs’ work is even more crucial. But it doesn’t stop short at fighting Staph A.
“We’re in the business of treating drug-resistant infections,” he said. “There are implications for our work that go beyond MRSA. We can take the results of our research and apply them to other infections.”
Heinrichs says the ability to collaborate with other researchers in the Facility will allow for a cross-pollination of ideas, which could lead to novel discoveries.
“One of the great things about the ImPaKT Facility is that it brings some of our nationally recognized experts in imaging and merges them with nationally recognized experts in pathogen-host interaction,” he said. “We have imagers working together with microbiologists in innovative collaborations to ask and answer new questions.”
For his graduate trainees, working in a high-level, multimodality facility and learning in an interdisciplinary environment is the perfect setting to prepare the next generation of research innovators.
“They’re burgeoning experts in microbiology, and now we put them in the lab with imagers,” Heinrichs said. “They will see the possibilities are almost endless in what they can do when merging these two fields.”