Puff. Puff. Pass.
 Photography by Ruslan Alekso via Pexels
Photography by Ruslan Alekso via Pexels
At the crossroads of teen culture and technology lies vaping – a health crisis that few are paying attention to, and fewer still understand. At Schulich Medicine & Dentistry, researchers are attempting to deconstruct this phenomenon and its impact on the health of our youth.
At a basketball court in the heart of London, Ont., a late afternoon game is underway.
The rhythmic thud of the ball, punctuated by the squeak of sneakers and the gasp of laboured breaths, echoes through the air.
Suddenly, a wispy plume of vapour rises from the corner, silencing the court.
Heads turn. The tricksters have arrived.
On the sidelines, a group of teens huddle together, eyes fixed on the ‘vape artists’ or ‘vaping tricksters,’ as they are known. The spectators watch in awe as the teen performers – their peers – exhale a dozen ‘O’ rings and jellyfish-shaped clouds of vapour that disappear into thin air leaving behind a lingering fruity residue.
The teens pass around a slim device, no larger than a USB stick, each taking turns to attempt the newly-learned ‘ghost inhale’ – inhaling, releasing and swiftly recapturing, drawing the vape cloud back into their mouths.
This spectacle of teens vaping is now all too familiar, not just limited to one basketball court, but seen at playgrounds, bus stops, schools, university campuses and mall entrances alike.
The hullabaloo over vaping
Vaping is essentially inhaling a fatty liquid, a concoction of one or more substances, commonly mistaken for ‘water vapour,’ using handheld electronic devices like e-cigarettes or vape pens. This mixture is super-heated by vape pens to vapourize substances, including nicotine, flavours and solvents. Beyond nicotine, vaping can be used to inhale aerosolized forms of cannabis, vitamins, melatonin, milk thistle and essential oils.
TEEN VAPING AT A GLANCE
17%
vaped in last 30 days
16%
used nicotine e-cigarettes
55%
find nicotine e-cigarettes easy to get
54%
vaped liquid cannabis
Source: Canadian Student Substance Survey 2021-22
Vapes and traditional cigarettes both deliver nicotine, but the critical distinction is their delivery mechanism: Vapes use heat to transform a nicotine liquid into an aerosol, where cigarettes contain tobacco leaves that are burned to generate smoke.
This difference, though seemingly minor, significantly impacts user experience and health outcomes, undermining vaping’s introduction as a harm reduction strategy.
“Vaping was initially promoted as a way to wean people off their nicotine dependency, gradually reducing their intake while mitigating the dangerous effects of tar and harmful toxins and carcinogenic substances associated with smoking,” said Jamie Seabrook, PhD, adjunct professor in the Departments of Epidemiology and Biostatistics and Paediatrics. “However, its perceived ‘cool’ factor and the allure of flavoured e-liquids soon captured a demographic it was never intended for – non-smokers and especially teenagers.”
The ease of use and sleek design of the devices, plus the false perception of vaping as a harmless activity have led to a concerning number of young people experimenting with these products, many of whom have never used nicotine before.
“The statistics are shocking,” said Seabrook, chair and professor in the School of Food and Nutritional Sciences at Brescia University College at Western University.
In a recent study conducted in collaboration with Evan R. Wiley from Schulich Medicine & Dentistry, Seabrook found 26 per cent – one in four – of Canadian high-school students had vaped in the previous month. Within this group, 12 per cent reported using vapes filled with nicotine exclusively. This study made national headlines, raising critical questions about policies and regulations around vaping in Canada.
According to statistics from the Canadian Student, Alcohol and Tobacco Survey, during 2006-2007, 12 per cent of grade 10 and 11 students reported smoking cigarettes. And while cigarette use has decreased since then, nicotine consumption has not, mainly attributed to vaping.
“The hypothesis is that the concentration of vape stores... is making the accessibility to vapes easier and influencing the prevalence of vaping among vulnerable populations, such as students and lower-income residents.”
—Jason Gilliland
Professor Jason Gilliland, PhD, and a team of researchers at his Human Environments Analysis Laboratory (HEAL) are working with Seabrook to better understand factors that draw teenagers to vaping.
They’re using various methods – from youth-focused surveys to leveraging big data – to understand the root causes of teen vaping, and to enable them to strategize appropriate prevention methods.
In 2021, Gilliland, professor in the Departments of Paediatrics and Epidemiology and Biostatistics, oversaw a unique student-led project to capture insights directly from young people. Named Teens Talk Vaping, the group’s mission was to understand why teenagers continue to vape, even when they are cognizant of the health hazards associated with it.
They conducted approximately 1,000 surveys and multiple focus groups with teens aged 13-19. They found most teens were introduced to vaping by their peers, purchasing vapes in stores was easy, and resources to quit, especially those that resonated with their age group, did not exist.
Gilliland and Seabrook are now turning their attention to the geographic distribution of vape stores within communities, examining how these businesses may disproportionately affect certain demographics.
“The hypothesis is that the concentration of vape stores in these specific locations is making the accessibility to vapes easier and influencing the prevalence of vaping among vulnerable populations, such as students and lower-income residents,” said Gilliland.
By understanding the location of vape stores and convenience stores where vapes are sold, the researchers hope to gain deeper insights into their potential influence on community health and socioeconomic disparities.
Playing catch-up
The world has witnessed a swift surge in the use of vaping products since they first hit the market in 2006. From simple devices to intricate, customizable ones, users can now choose between refillable and non-refillable cartridges or pods, a variety of vape liquids called ‘vape juice’ or ‘e-juice,’ as well as devices with adjustable power settings.
 Vaping products are booming in Canada.
Vaping products are booming in Canada.
(Eric Albrecht/The Columbus Dispatch)
“The Canadian market is booming with vape products – everything from innovative new flavours to different forms of nicotine,” said Jibran Khokhar, PhD, associate professor in the Department of Anatomy and Cell Biology and Canada Research Chair in Translational Neuropsychopharmacology at Schulich Medicine & Dentistry.
“Unlike traditional cigarettes, which burn continuously and contain accelerants to facilitate this, there is no unit measure (such as, cigarettes per day) with e-cigarettes. Instead, a dose of nicotine is available on demand and can be consumed discreetly.”
Khokhar’s research focuses on understanding the effects of substances like nicotine and cannabis on the brain, especially on the adolescent brain. What is unique about his research is that he simulates the real-world use of substances in his experimental designs with animal models. This involves mimicking not only the methods individuals use to ingest these substances, such as using vapes or edibles, but also factoring in real-world variables such as the strength of the substance consumed and even preferences among different genders.
By closely aligning the experiment conditions with real-world situations, he’s able to draw more accurate conclusions about the effects of substances on the developing brain.

“The vaping industry is an evolution of ‘big tobacco’ and may be using vaping to create future customers for combustible tobacco... And there are so many players in the market – local to international – we are struggling to even catch up.”
—Jibran Khokhar
In the absence of accurate data related to product trends and consumption patterns, Khokhar visits vape stores to monitor what’s available, observe customer preferences and assess new products on the shelf. Khokhar and his team even turn to social media platforms and online discussion threads to make sense of the teen vaping subculture.
“The vaping industry is an evolution of ‘big tobacco’ and may be using vaping to create future customers for combustible tobacco,” said Khokhar. “And there are so many players in the market – local to international – we are struggling to even catch up.”
Health Canada recently introduced Vaping Products Reporting Regulations to gather detailed information about the vaping product market, including product types and designs popular with Canadians, especially young people who vape, as well as to report ingredients in vaping substances.
“More data is needed to know whether tobacco control measures are working. And now with the legalization of cannabis, what are the multi-substance use trends among youth?” said Khokhar.
Khokhar’s research has found adolescents respond differently to e-cigarette vapour than adults. Using animal models, he found the adolescent brain finds nicotine vapour more rewarding compared to adult brains, even with shorter exposure durations, indicating a greater risk of nicotine addiction.
He has also found that even a single exposure to cannabis vapour can impact the brain, causing brain wave changes like those seen in schizophrenia, especially in regions involved with cognitive function. This is true even in individuals lacking risk factors for the illness, while having risk factors produces further impairments.
The researcher is now investigating the long-term effects of adolescent e-cigarette vapour exposure on behaviours linked to future combustible tobacco consumption and the brain mechanisms that make young people who vape more vulnerable to future smoking or cannabis use.
The worst-case scenario
In 2019, a local case of severe lung injury requiring intensive care was treated at London Health Sciences Centre (LHSC) in London, Ont.
The patient, a teen who had vaped for a brief period, experienced lung damage akin to what his physicians and researchers called ‘popcorn lung’ – a condition observed in microwave popcorn factory workers exposed to a chemical called diacetyl that inflames and damages the small airways in the lungs.

“Lungs have been designed to endure the extreme physical demands of everyday life. Because of this, symptoms don’t present during day-to-day activities until the damage is quite severe.”
— Grace Parraga
“We had not seen anything like that before,” said Grace Parraga, PhD, professor of Medical Biophysics and Canada Research Chair in Lung Imaging at Schulich Medicine & Dentistry. Parraga, whose research focuses on developing new imaging methods to measure small airway function in asthma and chronic obstructive pulmonary disease (COPD), quickly turned her attention to examining the lungs of vape users. Relying on a specialized MRI method that her team pioneered, research participants inhale a polarized gas that is visible in MRI scans. The team discovered crucial insights into both the destroyed airways and lung alveoli in damaged lung tissue among vape users.
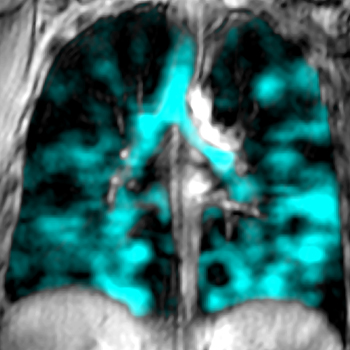 Image of a human lung damaged by vaping.
Image of a human lung damaged by vaping.
“Unlike young healthy lungs, young vaper lungs reveal widespread airway inflammation, obstruction and alveolar damage,” said Parraga. “Using an MRI, we could see that the inhaled gas did not fill the lung normally, revealing airways that were choked off and could not ventilate, revealing dark empty lung regions. In young asymptomatic vapers, these abnormalities cannot be detected using chest CT or pulmonary function tests.”
The sensitivity and sophistication of the state of-the-art lung imaging technology developed at Schulich Medicine & Dentistry also enabled Parraga to see the damage done to the tiny air sacs in the lungs and the fine tissue lining the air sacs – a place where an important exchange between oxygen and carbon dioxide happens.
“Lungs have been designed to endure the extreme physical demands of everyday life. Because of this, symptoms don’t present during day-to-day activities until the damage is quite severe,” said Parraga. “The new imaging technology is helping us more deeply understand what’s actually going on.”
The way forward
The first case of lung injury linked to vaping use, identified by Professor Dr. Karen Bosma and her colleagues at LHSC, sounded an alarm about the potential extent of harm vaping can inflict. Now London is quickly becoming the epicenter of vaping research in the country, as a diverse array of experts are banding together across disciplines to elucidate the wide range of health effects of vaping. For most scientists, it’s not just the worst-case scenario that’s worth studying: They insist that even seemingly minor effects of vaping on the body are a matter of concern.
“There’s an entire generation of vape users arising, and our health-care system isn’t equipped for this.

“There’s an entire generation of vape users arising, and our health-care system isn’t equipped for this.
— Ruud A. Veldhuizen
There’s not much research on the long-term effects, and we don’t completely understand how vaping and the substances and chemicals it involves impact our health,” said Ruud A. Veldhuizen, PhD, associate professor in the Department of Physiology and Pharmacology.
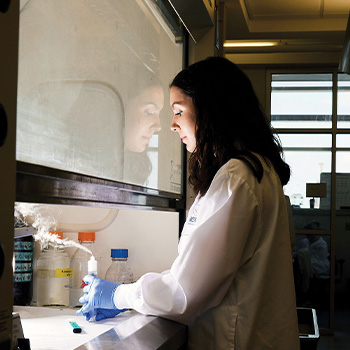 A typical research vaping session.
A typical research vaping session.
Veldhuizen’s Lung Lab focuses on studying pulmonary surfactant – a substance that facilitates the smooth inflation and deflation of the lungs with each breath by reducing surface tension and increasing lung stability. Now, they are using years of research to comprehend the nature of injuries caused by vape aerosols and develop potential treatments to address or reverse the damage.
“When e-cigarette aerosol is inhaled, it first and most crucially interacts with the pulmonary surfactant in the small airways and alveoli,” Veldhuizen explained. “We wanted to investigate whether the vapour affects its lung function.”
To do this, they placed a surfactant film inside a syringe and used a vaping device to force aerosol into the syringe. This process was repeated 30 times to simulate the inhaling and exhaling activity during a typical vaping session. Their findings indicated the e-liquid alone, even without nicotine or any other substance, when heated and inhaled as vapour, had noticeable effects on the surfactant.
The team also examined several types of vaping devices, flavours, additives, and nicotine, discovering that some flavours, such as menthol e-liquid, caused more damage to the surfactant.
Veldhuizen emphasized the need for understanding the unique health needs of vape users, especially when the lung gets challenged, such as during air quality advisories, following COVID-19 infection or during exercise.
“When vape users present with any other health issues, it’s important to know what the underlying problems are. Does being a vape user alter the scenario? How should we respond to the health needs of vape users? These are the questions we need to answer,” said Veldhuizen.
Time is short
Meanwhile, as the sun sets on the basketball court, the players plan their next move. Their rules are fluid, as ever-changing as the vaping phenomena the researchers are attempting to grasp. The clock is ticking, the game is on.








