Schulich Ivey Quality in Healthcare Consultancy
The Schulich Ivey Quality in Healthcare Consultancy is an innovative partnership between the Schulich School of Medicine and Dentistry and the Ivey School of Business at Western University. This ground-breaking course brings together healthcare providers and Honours Business Administration students in a co-learning environment to jointly investigate gaps in clinical care using quality improvement methodology.
The 24-week course format consists of four Ivey business students paired with one healthcare professional to explore how a healthcare issue can be optimized both from a financial and clinical perspective. The course combines invited speakers, coaching, and project work over the academic year. Notable projects the course has fostered over past years include reducing length of stay post-liver transplant saving the healthcare system $540,000 yearly (2019), developing a policy (i.e., resource stewardship) on the use of IV iron and what formulation to use (2020) and increasing the number of transcatheter aortic valve implantations (TAVIs) that were done per week by reducing inefficiencies and reallocating resources (2021).
The inter-hospital and cross departmental partnerships have fostered numerous relationships benefiting participants, payers, the healthcare system and most importantly, patients.
Visit the course website to learn more
Course Directors

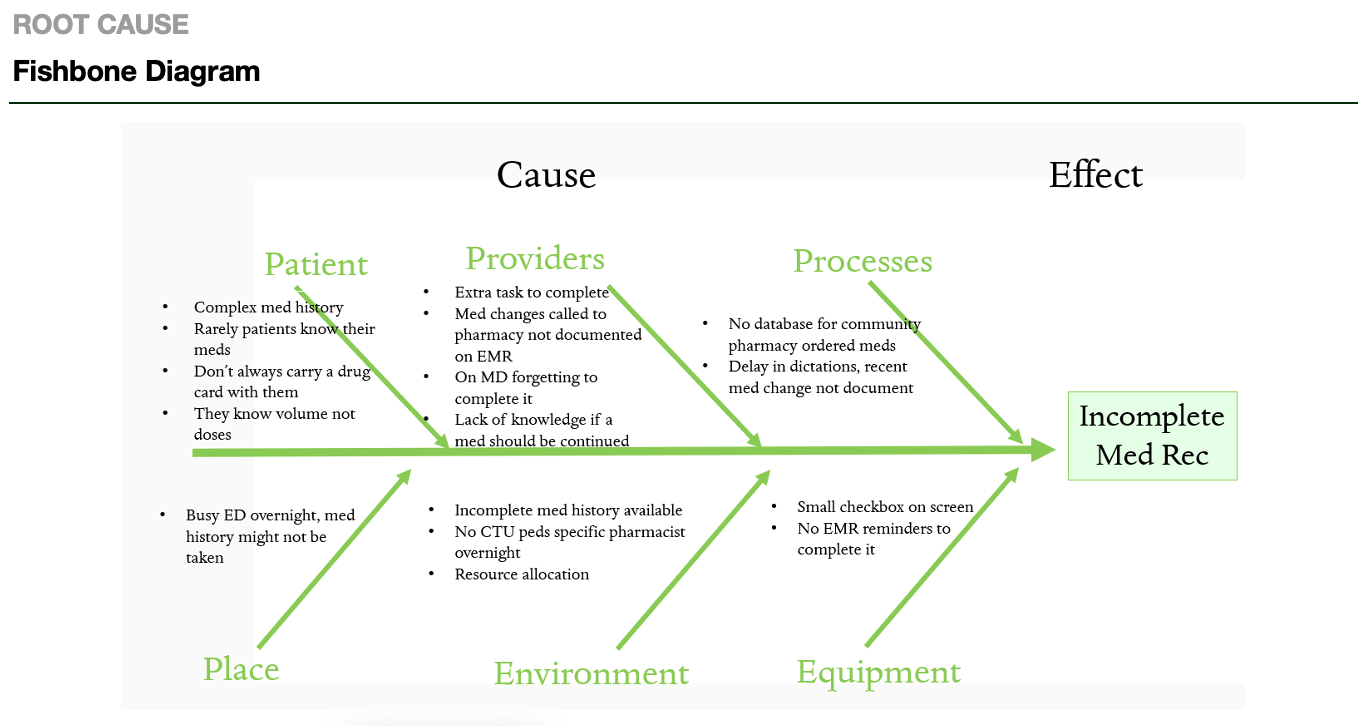 |
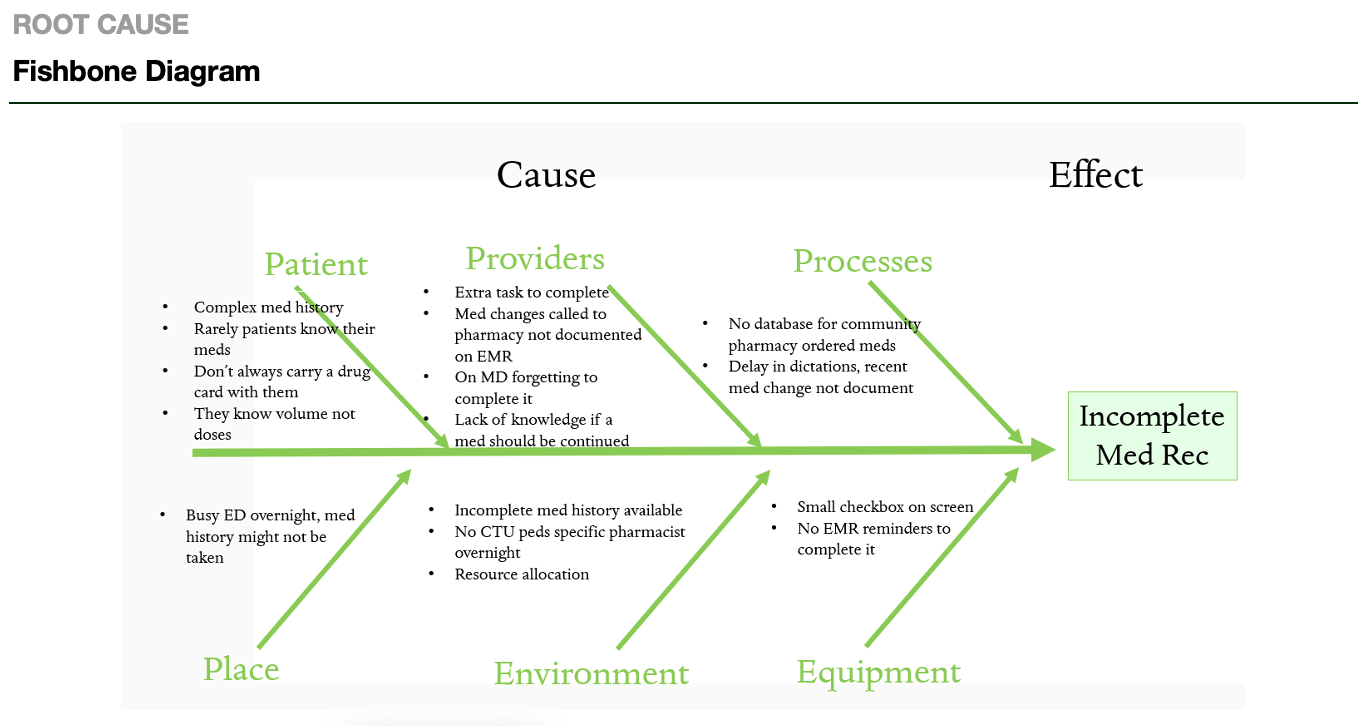
Improving Medication Reconciliation Rate at Admission to Paediatric Inpatient Medicine
AIM Statement: Improve medication reconciliation for inpatient pediatrics to 80% completion rate by April 2022.
Claire Hallsworth, Shawn Hu, Jennifer Wong, Dr. Farah Abdulsatar
|
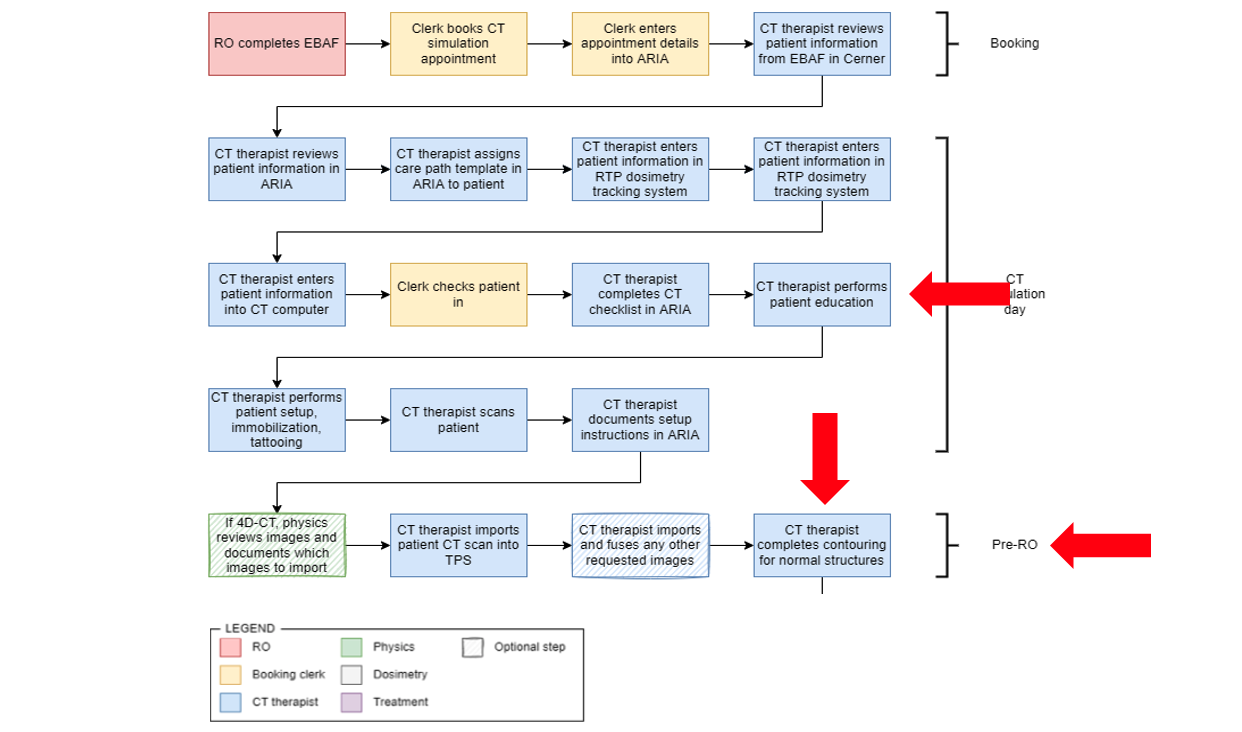 |
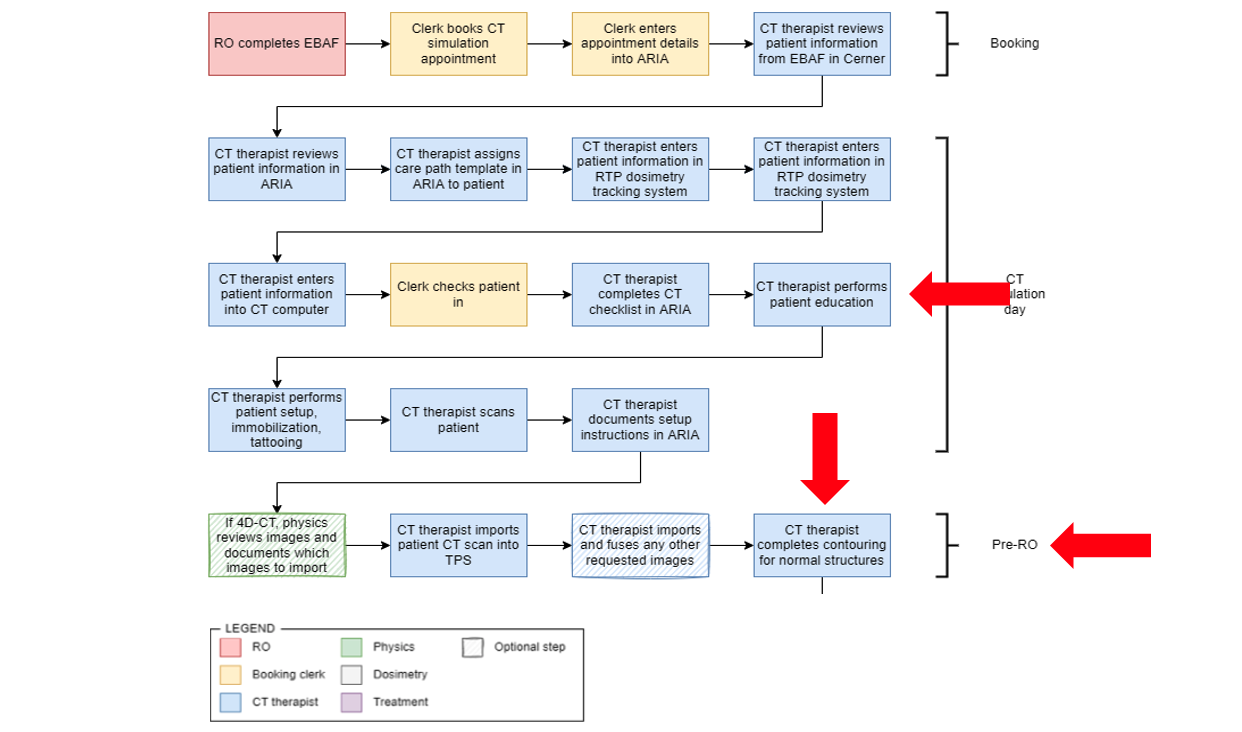
Decreasing wait times for radiation therapy
AIM Statement: By September 2022, for patients requiring radiation at LRCP, increase the number of patients that are simulated from 18 to 23 per day.
Angela Mao, Zuha Pathan, Zeba Rizvi, Alida Teodorescu, Dr. Andrew Arifin
|
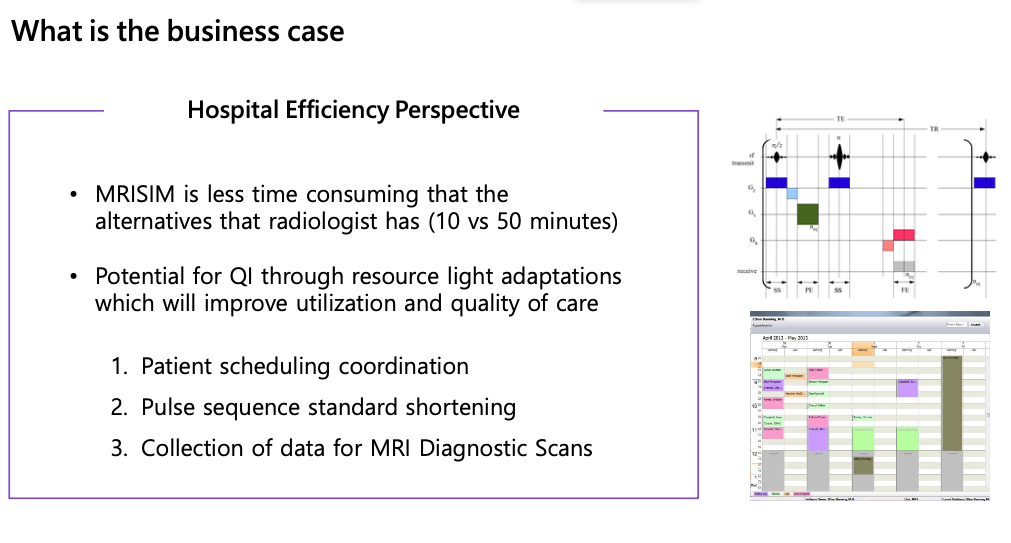 |
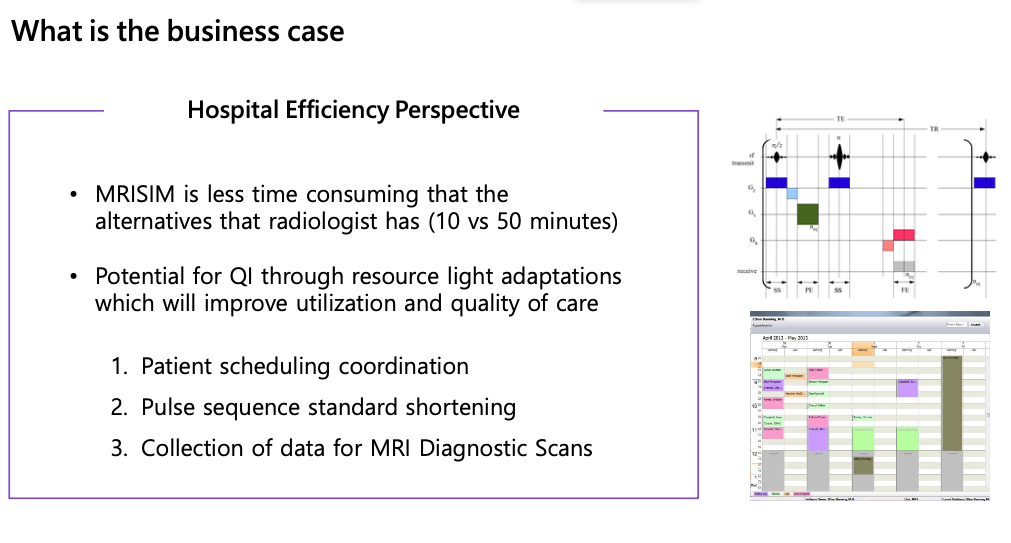
Improving Access to MRI for Treatment and Diagnosis - THIRD PRIZE WINNER
AIM Statement: By June 30th, 2022, for patients referred to the London Regional Cancer Program, increase the utilization of magnetic resonance imaging for radiotherapy treatment planning by 10% to meet accepted clinical practice standards.
Gaurav Chahal, Aliaa Abdelmeguid, Mila Gracic, Rachel Bai, Dr. Robert Dinniwell
|
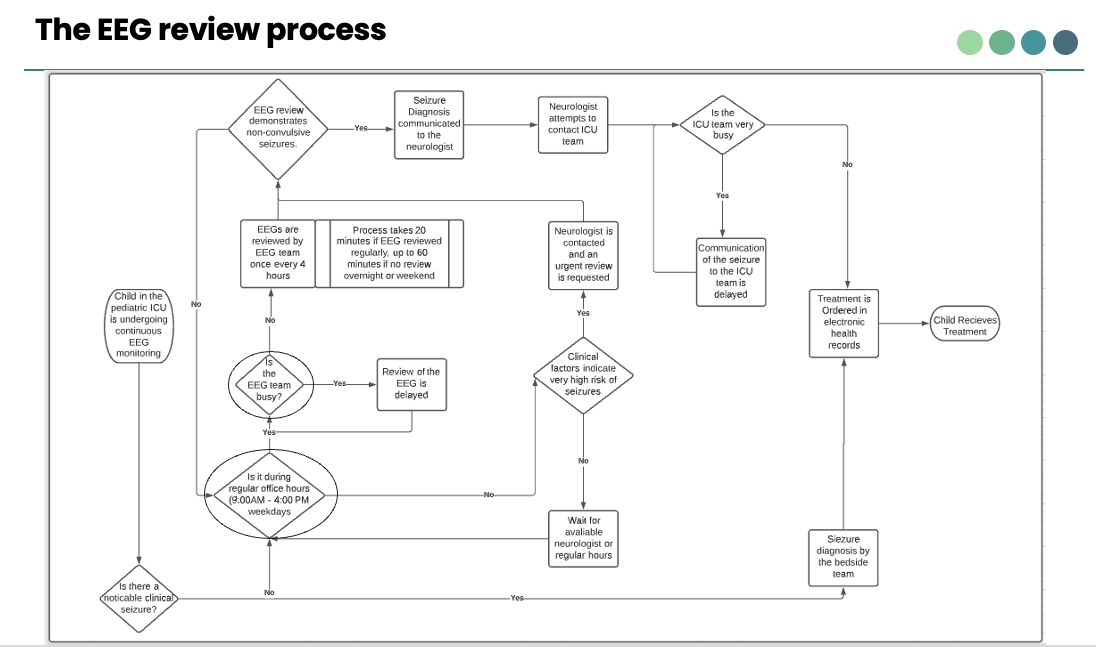 |
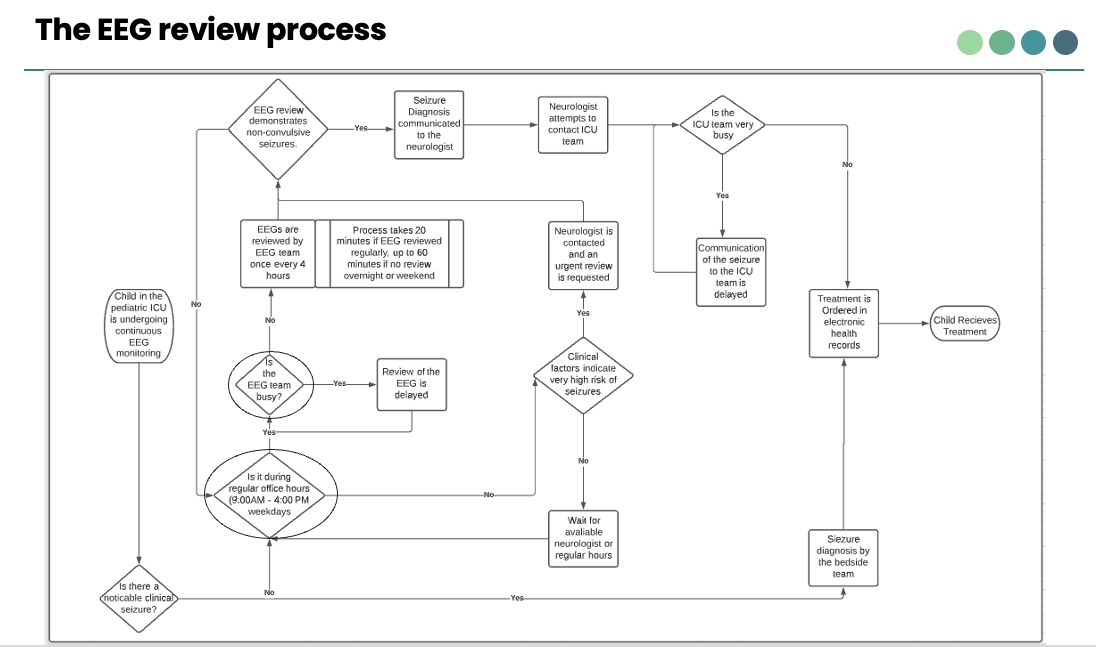
Enhancing timeliness of seizure diagnosis in critically ill children - FIRST PRIZE WINNER
AIM Statement: Within the next 2 years, increase the rate of timely diagnosis (within 1 hour) of seizures in critically ill children from < 25% to > 80% using simplified brain wave trends.
Celeste Alaimo, Adam Lampert, Gabriel Mancuso, Aimee Nguyen, Dr. Rishi Ganesan
|
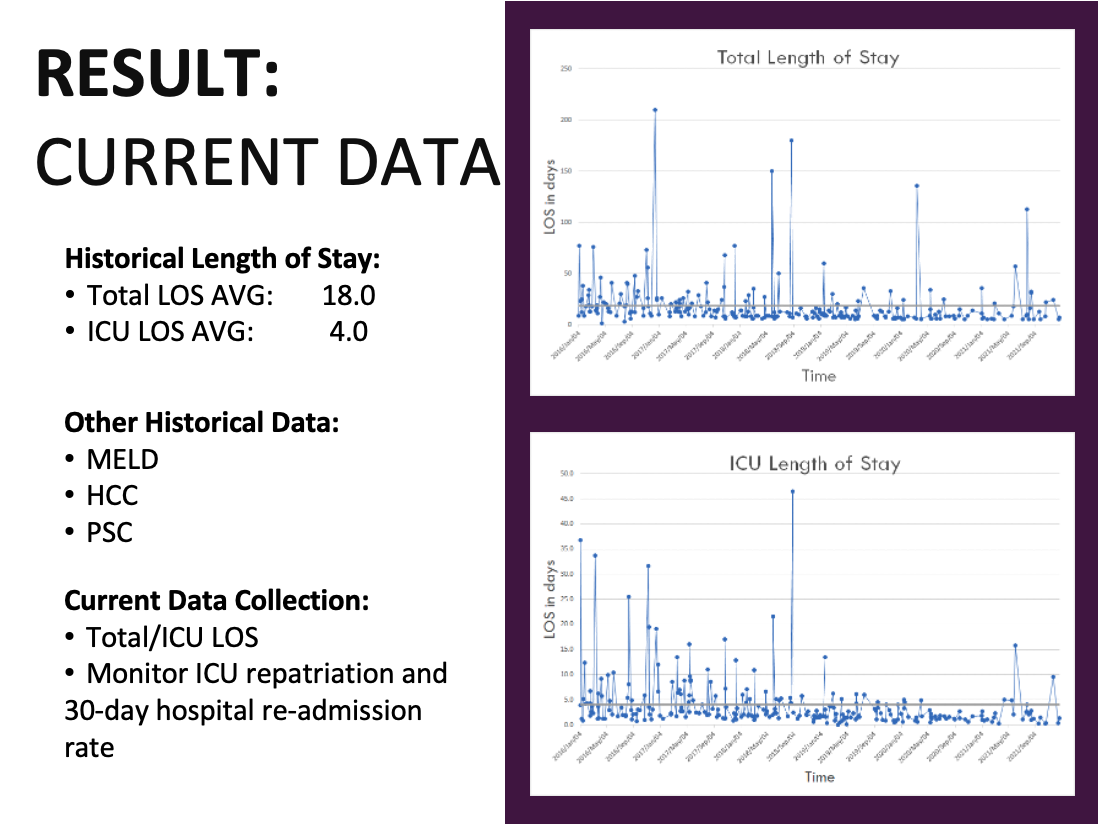 |
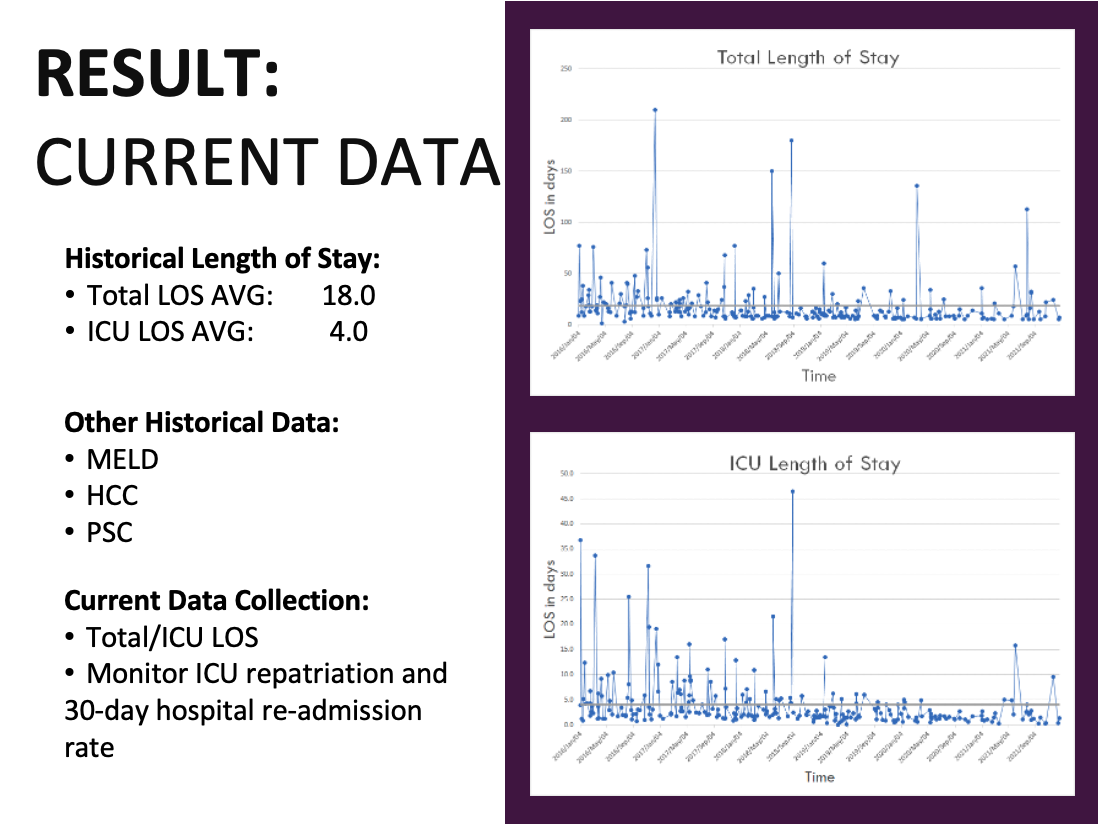
Liver Transplant Accelerated Recovery Program - SECOND PRIZE WINNER
AIM Statement: By December 2022, for cases undergoing Liver Transplants at LHSC, have 5-10% of patients successfully complete the Liver Transplant Accelerated Recovery Program.
Caroline Parson, Michael Lee, Kathryn Beri, Jasmine Yu, Dr. Nelson Gonzalez
|
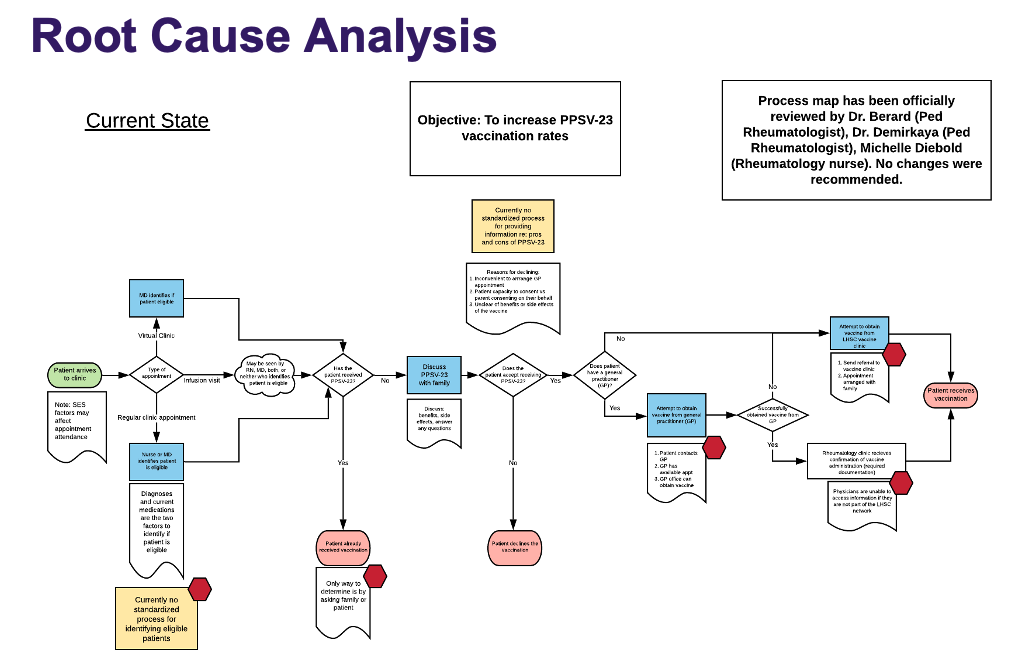 |
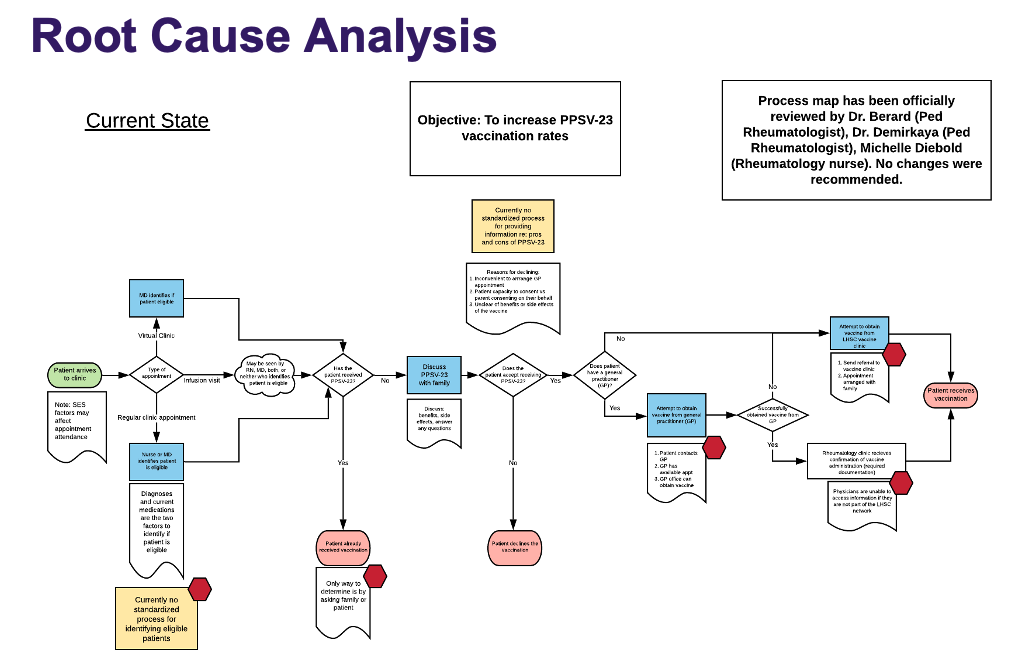
Increase PPSV-23 Vaccination Rates in Southwestern Ontario for Pediatric Rheumatology Patients
AIM Statement: By March 2022, increase the immunization rate of PPSV23 in pediatric rheumatology patients eligible for a publicly funded dose and followed at LHSC from 0% to 33%.
Aanya Bhatia, Cody Hudson, Flora Huang, Rebecca Lundrigan, Dr. Jonathan Park
|
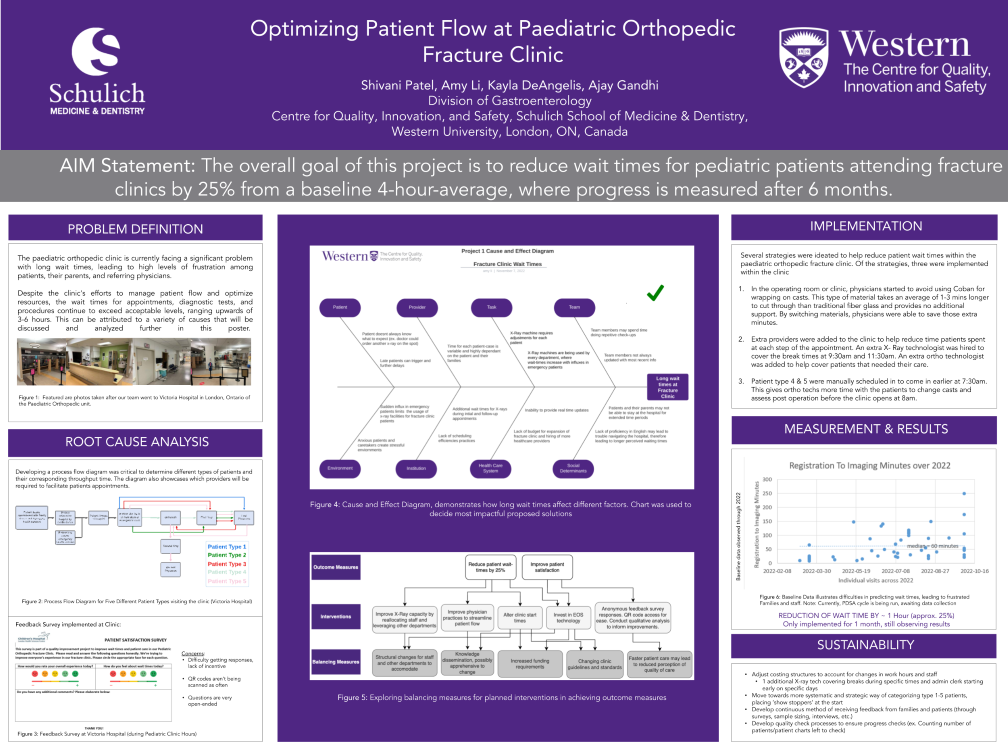 |
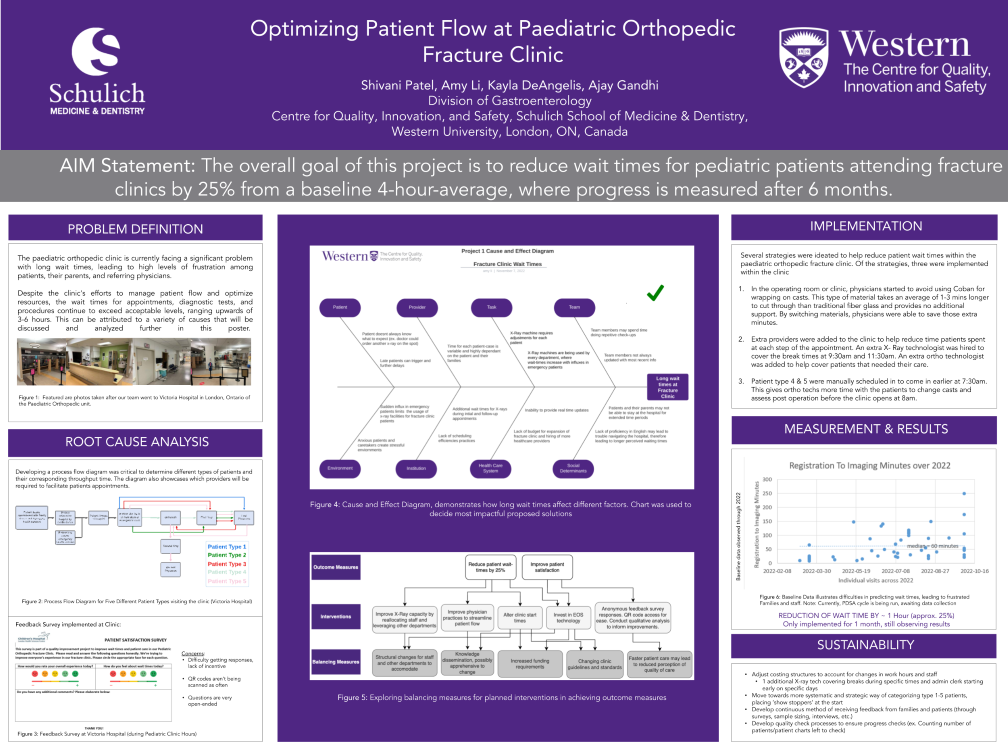
Optimizing Patient Flow at Paediatric Orthopedic Fracture Clinic
AIM Statement: The overall goal of this project is to reduce wait times for pediatric patients attending fracture clinics by 25% from a baseline 4-hour-average, where progress is measured after 6 months.
Shivani Patel, Amy Li, Kayla DeAngelis, Ajay Gandhi, Drs. Ryan Katchky, Ian Laxdal, Silvio Ndoja
|
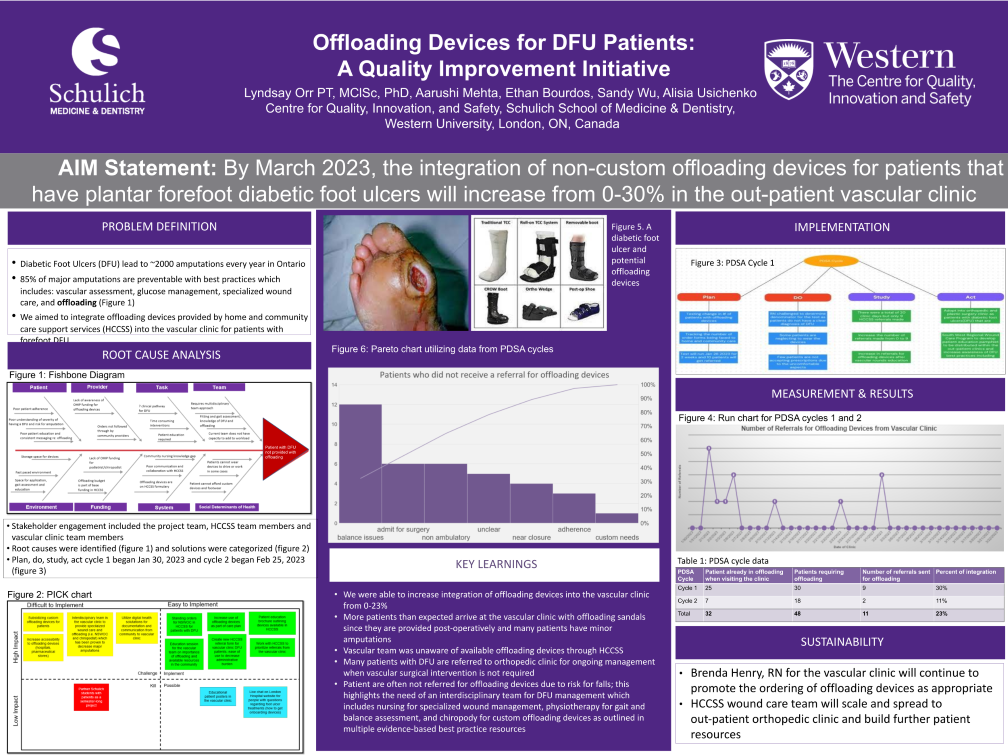 |
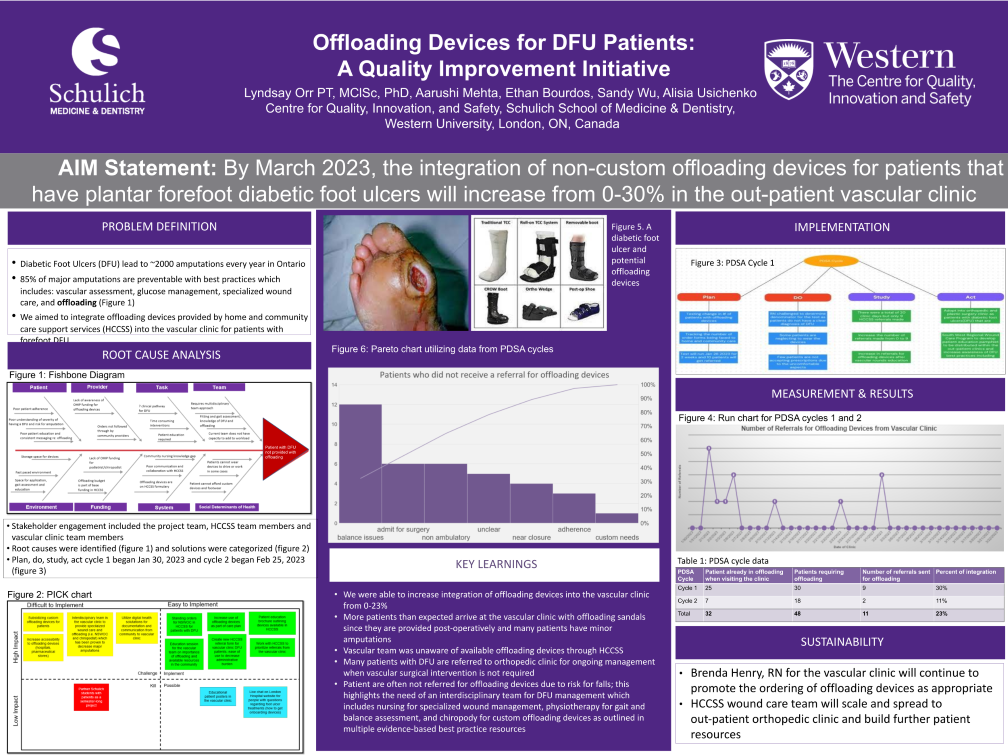
Offloading Devices for DFU Patients: A Quality Improvement Initiative
AIM Statement: By March 2023, the integration of non-custom offloading devices for patients that have plantar forefoot diabetic foot ulcers will increase from 0-30% in the out-patient vascular clinic.
Aarushi Mehta, Ethan Bourdos, Sandy Wu, Alisia Usichenko, Dr. Lyndsay Orr
|
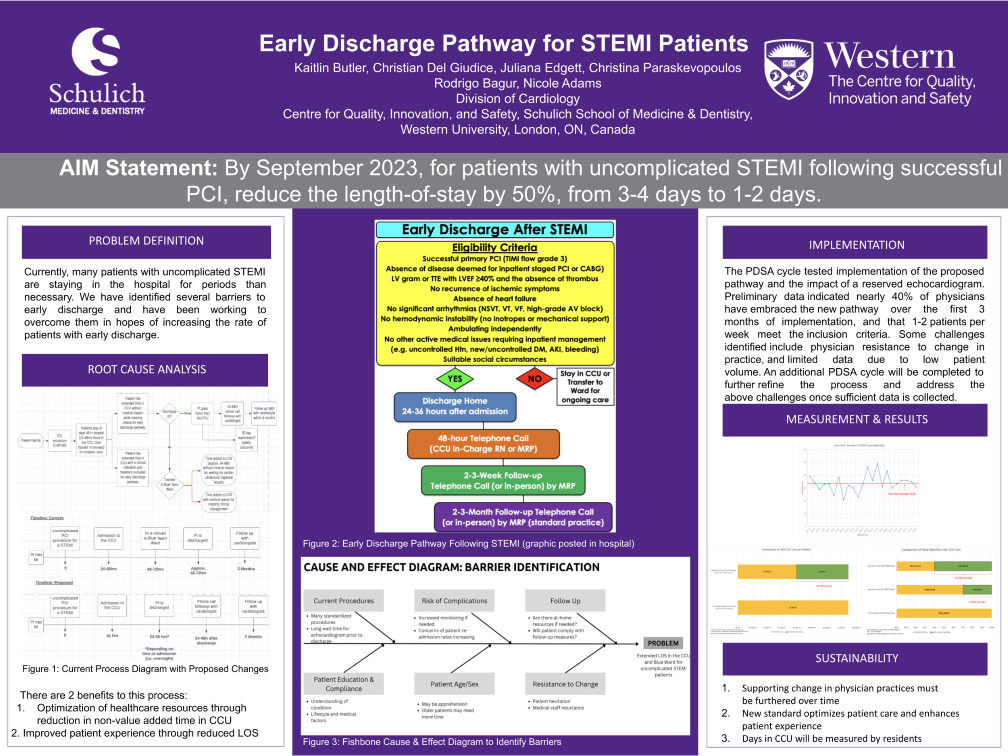 |
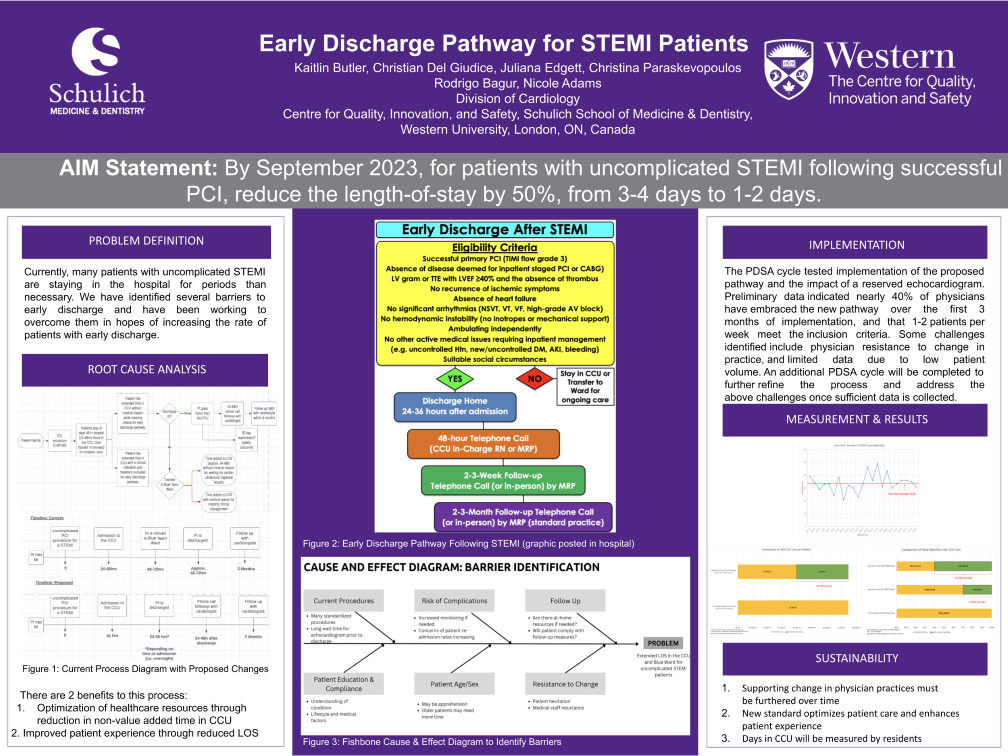
Early Discharge Pathway for STEMI Patients - THIRD PRIZE WINNER
AIM Statement: By September 2023, for patients with uncomplicated STEMI following successful PCI, reduce the length-of-stay by 50%, from 3-4 days to 1-2 days.
Kaitlin Butler, Christian Del Giudice, Juliana Edgett, Christina Paraskevopoulos, Dr. Rodrigo Bagur, Nicole Adams
|
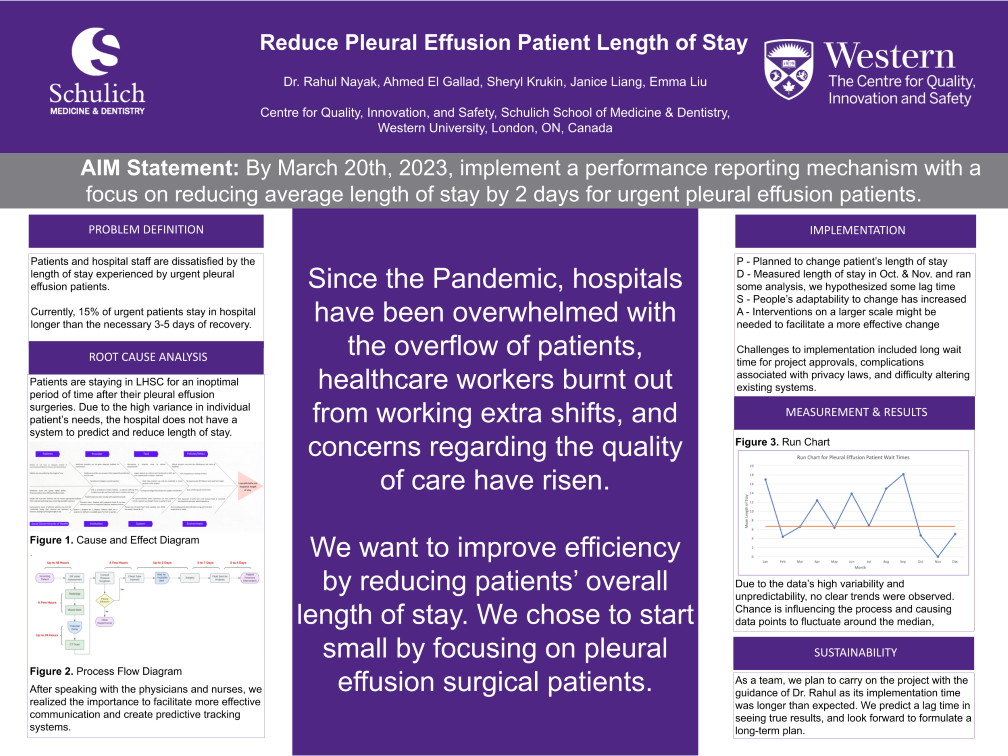 |
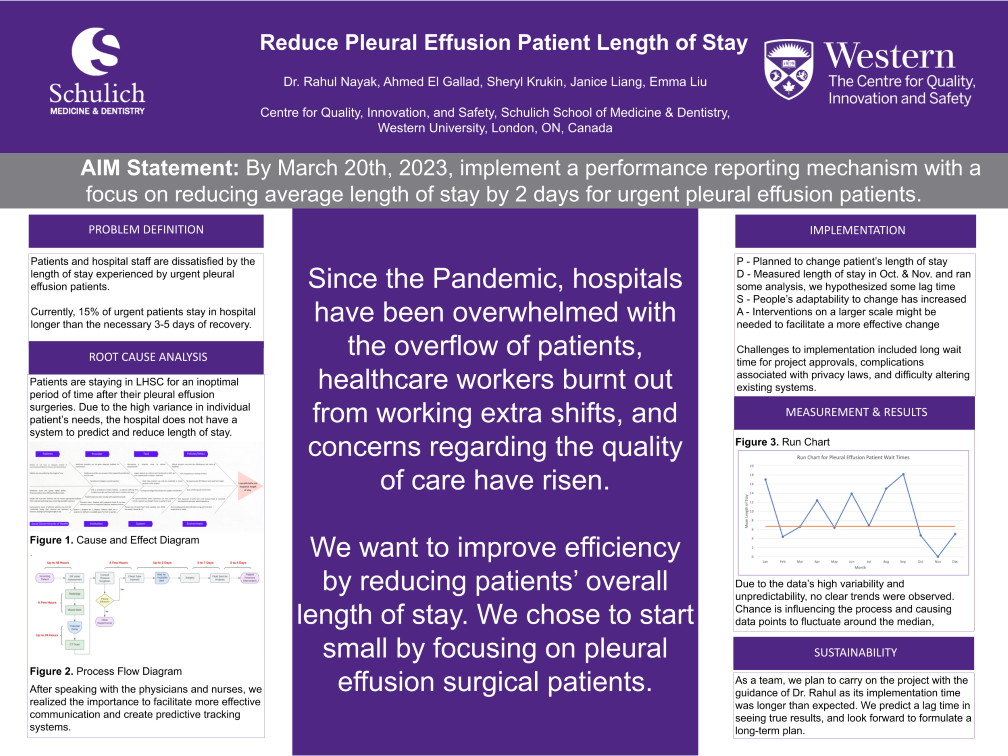
Reduce Pleural Effusion Patient Length of Stay
AIM Statement: By March 20th, 2023, implement a performance reporting mechanism with a focus on reducing average length of stay by 2 days for urgent pleural effusion patients.
Ahmed El Gallad, Sheryl Krukin, Janice Liang, Emma Liu, Dr. Rahul Nayak
|
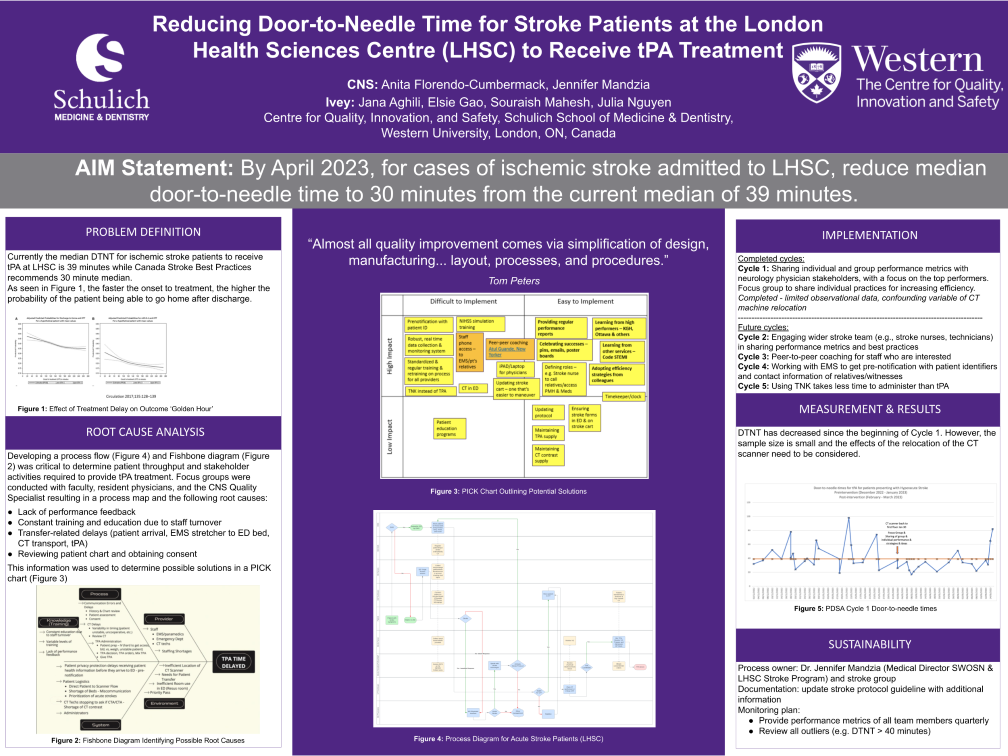 |
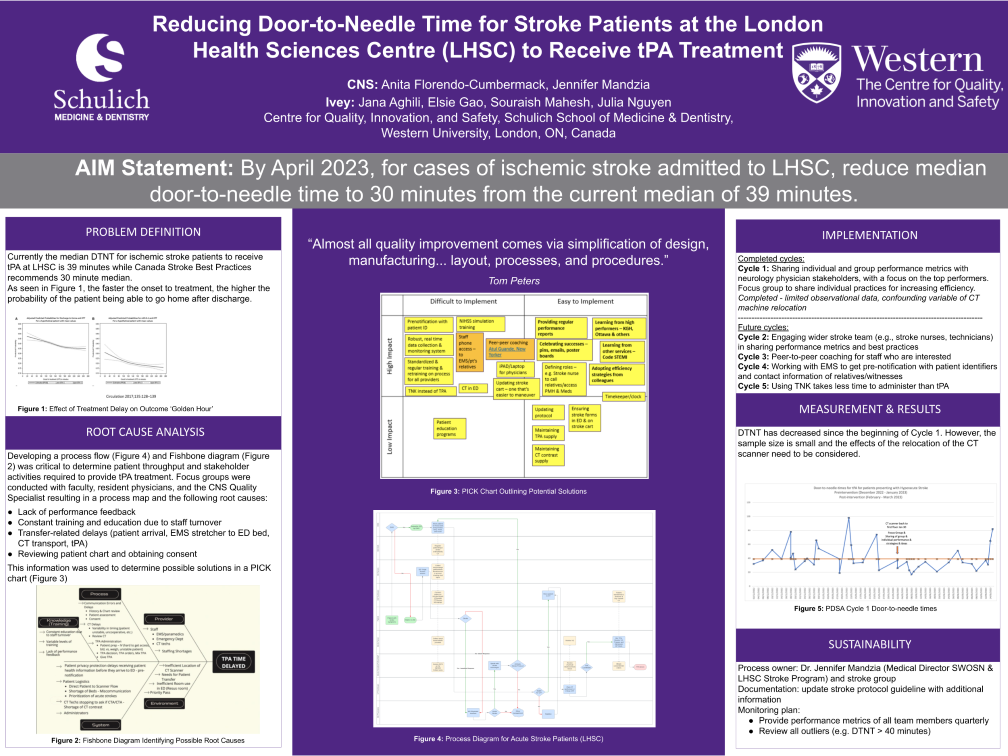
Reducing Door-to-Needle Time for Stroke Patients at the London Health Sciences Centre (LHSC) to Receive tPA Treatment - FIRST PRIZE WINNER
AIM Statement: By April 2023, for cases of ischemic stroke admitted to LHSC, reduce median door-to-needle time to 30 minutes from the current median of 39 minutes.
Jana Aghili, Elsie Gao, Souraish Mahesh, Julia Nguyen, Dr. Anita Florendo-Cumbermack, Jennifer Mandzia
|
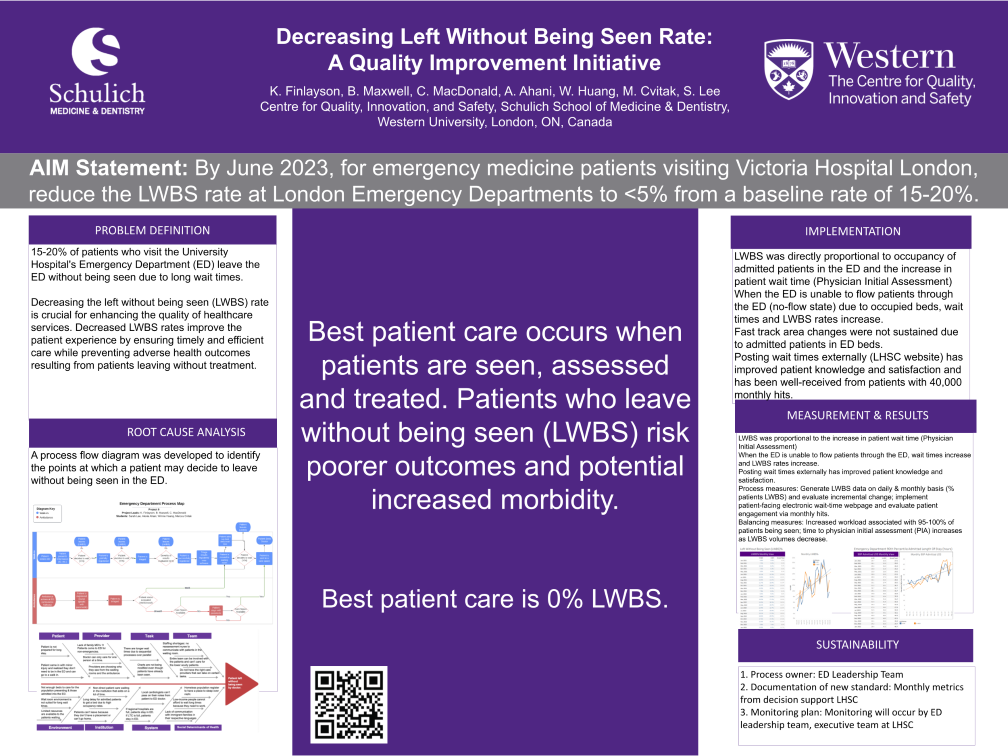 |
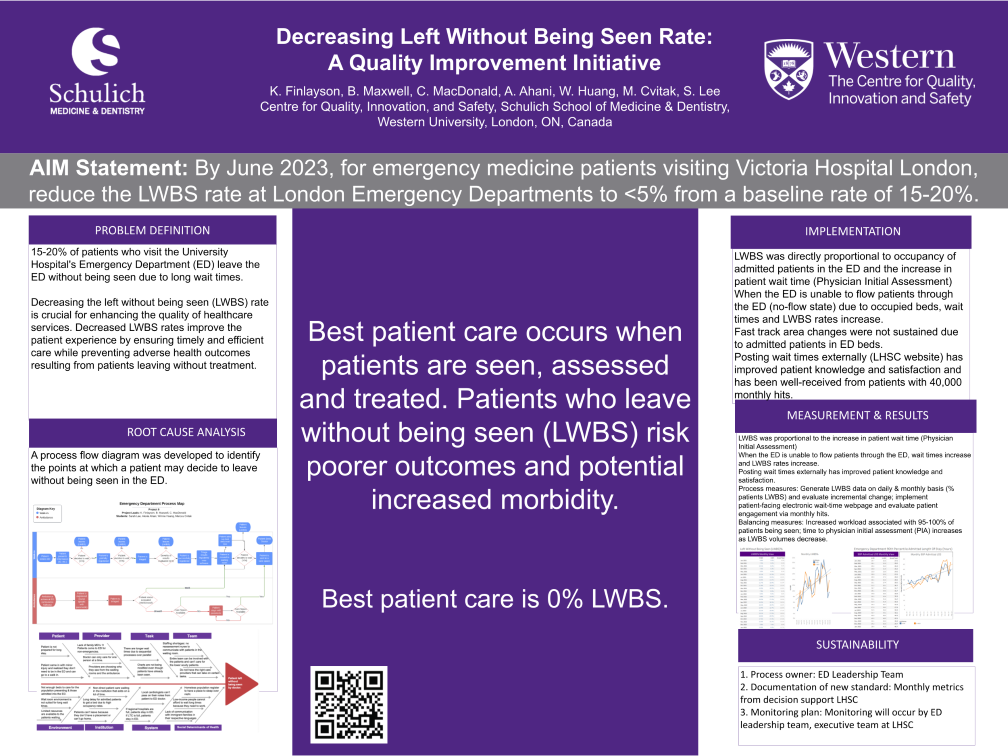
Decreasing Left Without Being Seen Rate: A Quality Improvement Initiative - SECOND PRIZE WINNER
AIM Statement: By June 2023, for emergency medicine patients visiting Victoria Hospital London, reduce the LWBS rate at London Emergency Departments to <5% from a baseline rate of 15-20%.
Alexia Ahani, Winne Huang, Marcus Cvitak, Sarah Lee, Dr. Christie MacDonald, Dr. Brendan Maxwell, Kelly Finlayson
|