World AIDS Day: Top 5 Myths about HIV/AIDS
In the early 1980s, when unusually high rates of pneumocystis jirovecii pneumonia (PJP) and Kaposi’s sarcoma began to present in populations of young gay men, physicians and public health officials were left wracking their brains for a correlation between the cases. The situation became even more confusing when it was later discovered that injection drug users and heterosexual women, too, were affected by this mysterious illness.
Today, we recognize these incidences as the earliest documented cases of HIV/AIDS, and have a greater understanding of what the virus does, how transmission occurs and the steps that can be taken to detect and manage the illness. Stigma and a lack of understanding about the virus, however, are still alive and well, and are fuelled by misinformation.
Infectious disease expert Dr. Michael Silverman, Chair of Infectious Diseases at Schulich Medicine & Dentistry, discusses the top five myths associated with HIV/AIDS that he has encountered in his practice as a physician, health care administrator and scientist. 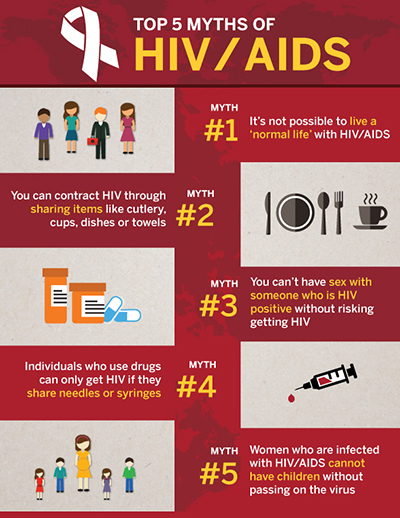 Myth 1: It is not possible to live a ‘normal’ life with HIV/AIDS
Myth 1: It is not possible to live a ‘normal’ life with HIV/AIDS
If an infected individual actively takes anti-retroviral medications, viral loads and the progression of the illness can be prevented.
“A lot of people think HIV/AIDS is a ‘death sentence’,” said Dr. Silverman. “An important point is that HIV/AIDS is eminently treatable. The treatments are well tolerated and most people have no side effects. As long as people get medical care and take their tablets, they can live a normal, healthy life.”
Myth 2: You can contract HIV through sharing items like cutlery, cups, dishes or towels
HIV cannot be transmitted through coming in contact with items used by individuals infected with HIV/AIDS. This is a widely debunked claim, but Dr. Silverman says people still avoid individuals with HIV/AIDS for fear of transmission.
“People fear catching HIV/AIDS from those who are infected, and so they avoid contact with them. This causes terrible stigma,” he said. “You cannot get HIV from sharing cutlery, cups, dishes or towels.”
Myth 3: You can’t have sex with someone who is HIV positive without risking getting HIV
Dr. Silverman says individuals infected with HIV who are also consistently taking medication and have an undetectable viral load cannot spread HIV through sex. This is referred to as ‘U =U’, or undetectable is untransmitable.
“People who are not infected with HIV can also take medications called PrEP, daily or prior to sex to dramatically reduce their risk. Finally, condoms remain very effective at reducing risk,” said Dr. Silverman.
Myth 4: Individuals who use drugs can only get HIV if they share needles or syringes
In addition to reusing needles to inject drugs, sharing drug preparation equipment, such as cookers and filters, can also cause HIV transmission. Research conducted by Dr. Silverman and others at Western University demonstrates that leftover material in drug preparation equipment can transfer viruses and bacteria between users, even when clean needles are used.
“The fact is that sharing drug preparation equipment, like cookers and filters, can also cause HIV transmission. This is a major problem in our community,” he said.
Myth 5: Women who are infected with HIV/AIDS cannot have children without passing on the virus
Otherwise known as vertical transmission, mother-to-child transmission of HIV is preventable. In Canada, with proper interventions during pregnancy, labour, delivery and breastfeeding, vertical transmission rates can certainly be reduced to less than one per cent and possibly reduced to zero.
“Vertical transmission between a mother and child is preventable,” said Dr. Silverman. “As long as the mother is tested early during pregnancy and put on medications, we should be able to prevent all babies from getting HIV.”
Dr. Michael Silverman, MD, FRCP, FACP, AAHIVMed, Chair of Infectious Diseases, Schulich School of Medicine & Dentistry at Western University.
Dr. Silverman completed his medical degree and residency in Internal Medicine at the University of Toronto. He carried out a fellowship in infectious diseases at the University of Manitoba in Winnipeg, and an HIV post-doctoral fellowship (1991- 1992) at the University of California, San Francisco, USA.
Dr. Silverman is currently Chair of Infectious Diseases at the Schulich School of Medicine at Western University; Chief of Infectious Diseases for London Health Sciences Centre and St. Joseph’s Hospital, London; Medical Director of the HIV Clinic, St. Joseph’s Hospital; Co-Director of Infection Control, London Health Sciences Center and St. Joseph’s Hospital; POEM Scientist in the Department of Medicine; Assistant Professor of Medicine and Infectious Diseases, Western University, Assistant Professor of Global Health, Dalla Lana School of Public Health, University of Toronto and Associate Member, School of Graduate Studies, University of Toronto.
Dr. Silverman established the Positive Care Clinic in Whitby, Ontario (the regional HIV/Hepatitis clinic) and the Durham Regional Tuberculosis Clinic in Ajax. Formerly, he has worked as a consultant in Infectious Diseases at Rouge Valley Hospital and Lakeridge Health. Dr. Silverman was also Director of Infection Control at the Henry Ford Hospital, in Detroit, Michigan from 2004 to 2005.
He has extensive experience conducting research and doing humanitarian medical relief in developing countries including Guyana, Zimbabwe, Zambia, Uganda and Thailand.








